
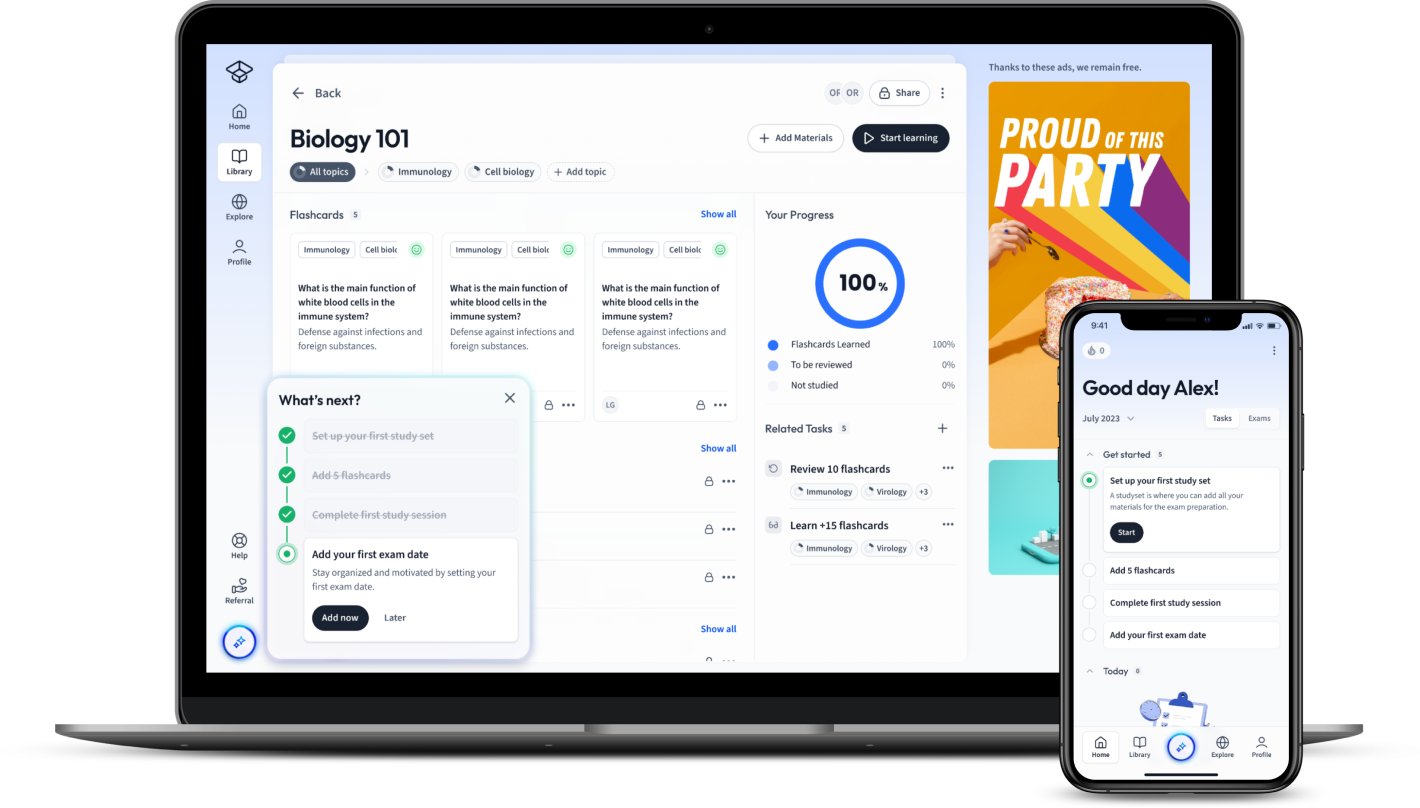
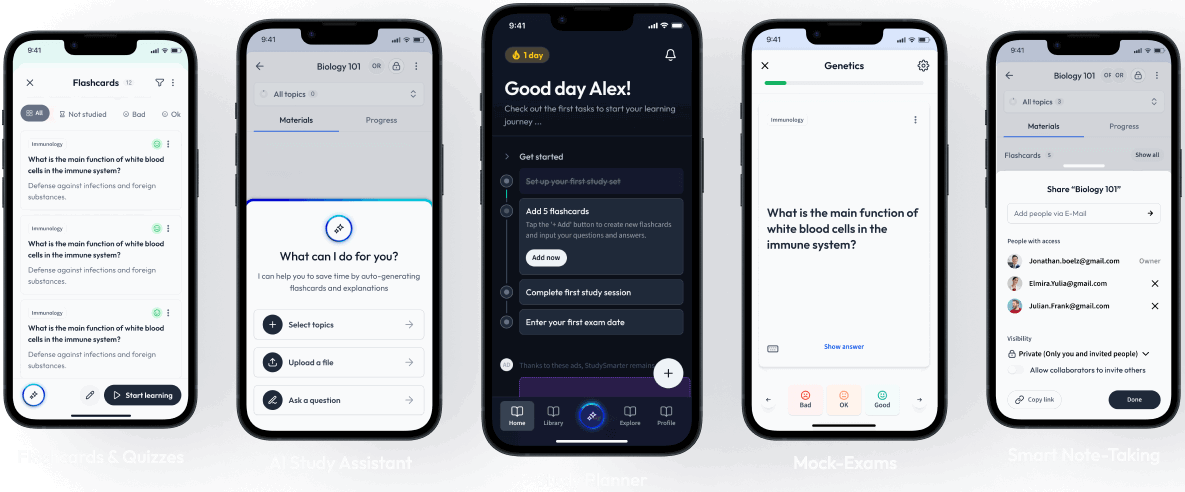
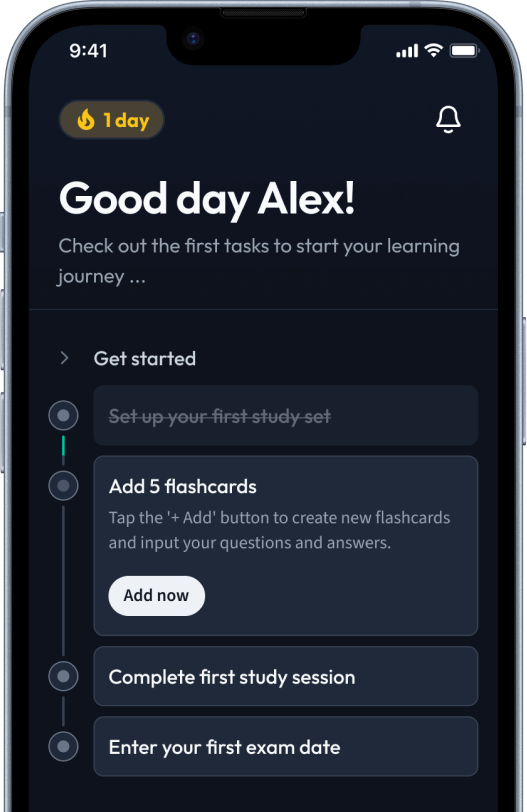
StudySmarter: Study help & AI tools
4.5 • +22k Ratings
More than 22 Million Downloads
Free
Diabetes is a chronic condition characterised by elevated levels of glucose in the blood, owing to the body's inability to produce or effectively use insulin. It divides into two main types: Type 1, where the immune system attacks insulin-producing cells, and Type 2, associated with lifestyle factors and genetics. Understanding the symptoms, management strategies, and potential complications of diabetes is crucial for maintaining health and preventing long-term damage.


Lerne mit deinen Freunden und bleibe auf dem richtigen Kurs mit deinen persönlichen Lernstatistiken
Jetzt kostenlos anmeldenDiabetes is a chronic condition characterised by elevated levels of glucose in the blood, owing to the body's inability to produce or effectively use insulin. It divides into two main types: Type 1, where the immune system attacks insulin-producing cells, and Type 2, associated with lifestyle factors and genetics. Understanding the symptoms, management strategies, and potential complications of diabetes is crucial for maintaining health and preventing long-term damage.
Diabetes is a chronic condition that affects the way the body processes blood sugar, known as glucose. Managing this condition is crucial because it involves a balance between diet, exercise, and medication. Understanding diabetes is the first step towards effective management and leading a healthy life.
Diabetes Mellitus is a group of metabolic diseases characterized by a high level of glucose in the blood over a prolonged period. The condition occurs when the pancreas cannot produce enough insulin or when the body cannot effectively use the insulin it produces. Insulin is a hormone that regulates blood sugar.
Diabetes Mellitus: A metabolic disorder that primarily impacts glucose metabolism, leading to higher than normal blood sugar levels.
Insulin acts as the key that allows glucose to enter the body's cells from the blood.
Understanding the different types of diabetes is essential for recognising the symptoms and managing the condition effectively. The main types include Type 1, Type 2, and Gestational Diabetes.
| Type | Description |
| Type 1 Diabetes | An autoimmune condition where the body attacks its own pancreas, reducing insulin production. |
| Type 2 Diabetes | The most common form, resulting from the body's ineffective use of insulin. |
| Gestational Diabetes | Occurs in pregnancy and can increase the risk of developing Type 2 diabetes later in life. |
Example: A person with Type 1 diabetes may need to inject insulin daily to manage their condition, while someone with Type 2 diabetes might initially manage their condition through lifestyle changes and medication.
It's also worth noting the existence of rare forms such as Monogenic Diabetes, which is a result of a mutation in a single gene and occurs in families. This highlights the complex and varied nature of diabetes.
Early detection of diabetes symptoms can lead to better management of the condition. Common symptoms include, but are not limited to, the following:
Example: If you, or someone you know, experiences persistent symptoms such as excessive thirst and a marked increase in the frequency of urination, it might be advisable to consult a healthcare professional for potential diabetes screening.
Diabetes is not a one-size-fits-all condition. Rather, it's a group of diseases that influence how the body uses blood glucose, vital for health because it's an important source of energy for the cells that make up muscles and tissues, as well as the brain's main fuel source. Understanding the different types of diabetes is key to unravelling the intricacies of this widespread condition.
Type 1 diabetes is an autoimmune condition that primarily affects children and young adults, but it can occur at any age. It's characterised by the pancreas's inability to produce insulin due to the immune system mistakenly attacking and destroying the insulin-producing beta cells.
Type 1 Diabetes: An autoimmune disease where the immune system attacks the pancreas, leading to little to no insulin production.
Managing Type 1 diabetes involves a carefully calculated balance of daily insulin administration, either through injections or an insulin pump, a healthy diet, regular physical activity, and frequent monitoring of blood glucose levels.
Type 2 diabetes is the most common form of diabetes and typically develops in adults over the age of 45 years, but is increasingly occurring in younger age groups including children, adolescents, and young adults. Unlike Type 1, Type 2 diabetes is often associated with excess body weight and physical inactivity.
Type 2 Diabetes: A metabolic disorder characterised by high blood glucose levels due to the body's inability to use insulin effectively.
Management strategies include lifestyle changes such as a balanced diet, regular exercise, and medication to help control blood sugar levels. In some cases, insulin therapy may become necessary. Monitoring and education are pivotal for effectively managing Type 2 diabetes and preventing complications.
Gestational diabetes occurs exclusively during pregnancy and resembles Type 2 diabetes in several ways. It affects how the cells use glucose, leading to high blood sugar that can affect the pregnancy and the baby's health. Most women with gestational diabetes can control their blood sugar levels with a balanced diet and exercise, but some may require insulin injections.
Gestational Diabetes: A form of diabetes that develops during pregnancy and usually disappears after giving birth.
Close monitoring of the blood sugar levels is essential throughout pregnancy to ensure the health of both mother and baby. After birth, most women's glucose level returns to normal, though they're at higher risk for developing Type 2 diabetes later in life.
Though not related to the more familiar types of diabetes Mellitus, Diabetes Insipidus is a rare condition that also affects the body's handling of fluids. It involves a disorder of salt and water metabolism, leading to excessive thirst and large quantities of urine.
Diabetes Insipidus: A rare disorder causing an imbalance of fluids in the body, resulting in intense thirst and the production of large amounts of urine.
This condition can be caused by problems with the kidney's ability to respond to Antidiuretic Hormone (ADH) or by the insufficient production of ADH by the pituitary gland. Treatment usually focuses on addressing the underlying cause and often includes medication and dietary changes to manage symptoms and prevent dehydration.
Living with diabetes requires an understanding of how to balance treatment with everyday life. Effective management includes monitoring blood glucose levels, adhering to a healthy lifestyle, and, when necessary, medication. Regardless of the type of diabetes, adopting a comprehensive approach helps in minimising complications and maintaining quality of life.Here's a closer look at managing the intricacies of diabetes across different scenarios:
Type 1 diabetes management is a delicate balance requiring constant monitoring to ensure blood glucose levels remain stable. The cornerstone of managing Type 1 diabetes includes:
Continuous glucose monitoring devices have significantly improved the way individuals with Type 1 diabetes can track their blood sugar levels in real-time.
For many with Type 2 diabetes, lifestyle adjustments serve as the first line of defence in managing the condition. Key changes include:
Example: Incorporating a daily 30-minute walk or other forms of physical activity can significantly benefit individuals with Type 2 diabetes by improving insulin sensitivity.
Gestational diabetes requires careful management to ensure the health of both mother and baby. Key strategies include:
Most women with gestational diabetes return to normal glucose levels after giving birth, but should still undergo diabetes screening at least every three years.
Diabetes treatment varies significantly across the spectrum, tailored to the individual's specific needs and type of diabetes. It ranges from dietary management and exercise for Type 2 diabetes to insulin therapy for Type 1. Moreover, advancements in medical technology such as insulin pumps and continuous glucose monitoring systems have vastly improved quality of life for individuals with diabetes.Innovations in diabetes treatment are constantly evolving, reflecting the need for personalised care plans that accommodate the unique circumstances of each individual living with diabetes.
Emerging research into beta-cell transplantation and the potential for closed-loop insulin delivery systems (also known as an 'artificial pancreas') promises a future where managing diabetes could become even more automated and tailored to individual needs, significantly reducing the burden of daily management for individuals with Type 1 diabetes.
Diabetic Ketoacidosis (DKA) is a serious and potentially life-threatening complication often associated with Type 1 diabetes, though it can also occur in Type 2 diabetes. It arises when the body produces high levels of blood acids known as ketones.This condition develops when your body can't produce enough insulin. Without insulin, your body begins to break down fat as fuel. This process produces a buildup of acids in the bloodstream known as ketones, leading to DKA if left untreated.
Diabetic Ketoacidosis (DKA): A severe complication of diabetes characterised by the excessive build-up of ketones in the blood, leading to acidosis.
Example: A patient forgetting to take their insulin could experience high blood sugar levels, leading to the breakdown of body fat for energy and a subsequent accumulation of ketones, triggering DKA.
Symptoms of DKA include nausea, vomiting, abdominal pain, rapid breathing, and, if untreated, can progress to diabetic coma.
Glucose, a simple sugar, is the primary energy source for the body's cells. In people with diabetes, this essential process is disrupted. The pancreas either doesn't produce enough insulin or the body can't effectively use the insulin it does produce, leading to elevated levels of glucose in the blood—a condition known as Hyperglycaemia.Regular monitoring of blood glucose levels is crucial for individuals with diabetes to prevent complications such as nerve damage, kidney disease, and vision problems.
Hyperglycaemia: A condition characterised by higher than normal levels of glucose in the blood, often associated with diabetes.
Eating a balanced diet, regular exercise, and medication can help manage blood sugar levels effectively.
Monitoring glucose levels in urine is another method used to manage diabetes. While the kidneys typically reabsorb glucose and prevent it from entering the urine, elevated blood sugar levels can cause glucose to be excreted.This condition, known as glucosuria, can be an indicator of unmanaged or poorly controlled diabetes. Regular urine tests can help monitor the effectiveness of diabetes management strategies, aiding in the adjustment of treatment plans to better regulate blood sugar levels.
Glucosuria: The excretion of glucose in the urine, typically a symptom of uncontrolled diabetes.
Example: After consuming a large meal, a person with diabetes might find their glucose levels spike, leading to the presence of glucose in their urine—signalling the need to adjust their insulin dosage.
Although the presence of glucose in urine can indicate high blood sugar levels, the lack of it is not a reliable indicator of well-controlled diabetes. This emphasises the importance of regular blood glucose monitoring alongside urine tests for a comprehensive understanding of an individual's diabetes management.
What is type I diabetes characterised by?
Type I diabetes is an acute onset, usually before 30 years of age. It also includes the destruction of the pancreatic beta cells.
What is type II diabetes characterised by?
Type II is more commonly seen in adults over 30-40 years of age. Insensitivity of insulin receptors on the tissue cells to insulin followed by impaired insulin secretion.
How is the type I diabetes controlled?
Insulin injections, having a healthy lifestyle, and diet control type I diabetes.
How is type II diabetes controlled?
Low carbs and high fibre diet. Increased physical activity. Treatment may be supplemented by insulin injections, drugs that increase insulin secretion in the body, and/or drugs that reduce glucose absorption in the gut.
Why is it important to filter the content of the test tubes after reaction with Benedict’s solution?
The reaction produces a white precipitate that may interfere with light absorbance and hence result in inaccurate data.
What are the early signs of diabetes?
Individuals with diabetes often complain of tiredness, and increased thirst and hunger. They also show signs such as hyperglycaemia, presence of glucose in their urine (glycosuria), urinating excessively (polyuria), regular episodes of thrush, weight loss and blurred vision.
Already have an account? Log in
Open in AppThe first learning app that truly has everything you need to ace your exams in one place
Sign up to highlight and take notes. It’s 100% free.
Save explanations to your personalised space and access them anytime, anywhere!
Sign up with Email Sign up with AppleBy signing up, you agree to the Terms and Conditions and the Privacy Policy of StudySmarter.
Already have an account? Log in