
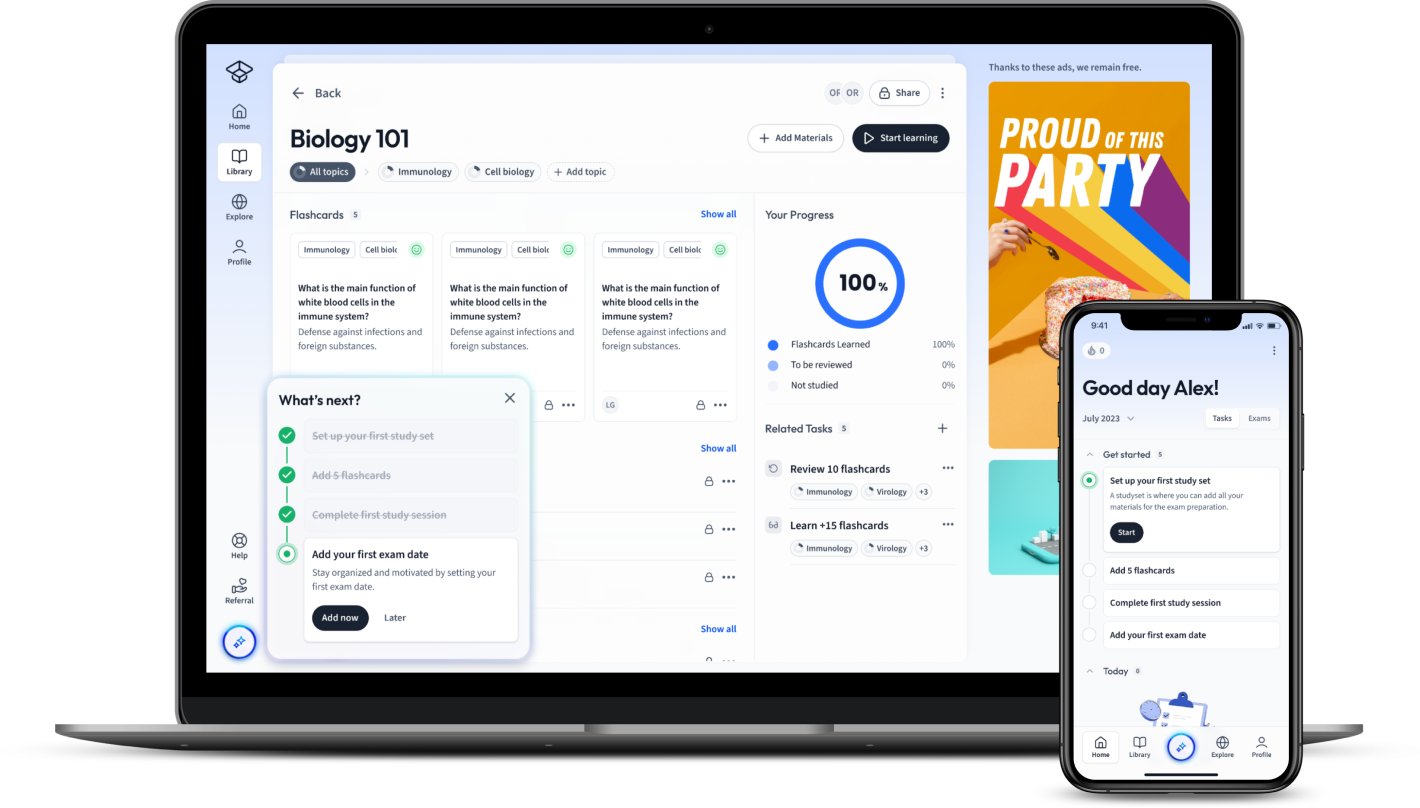
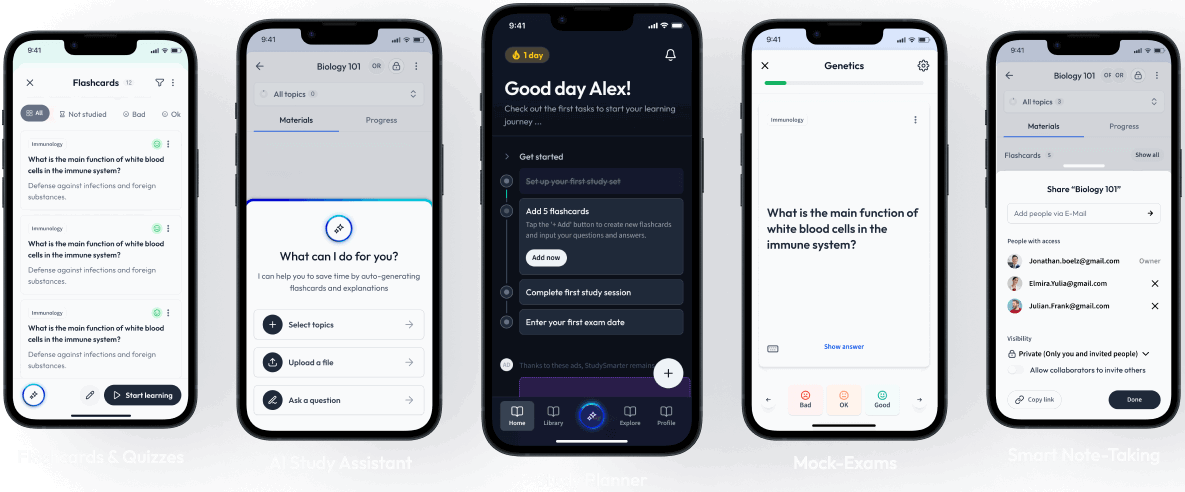
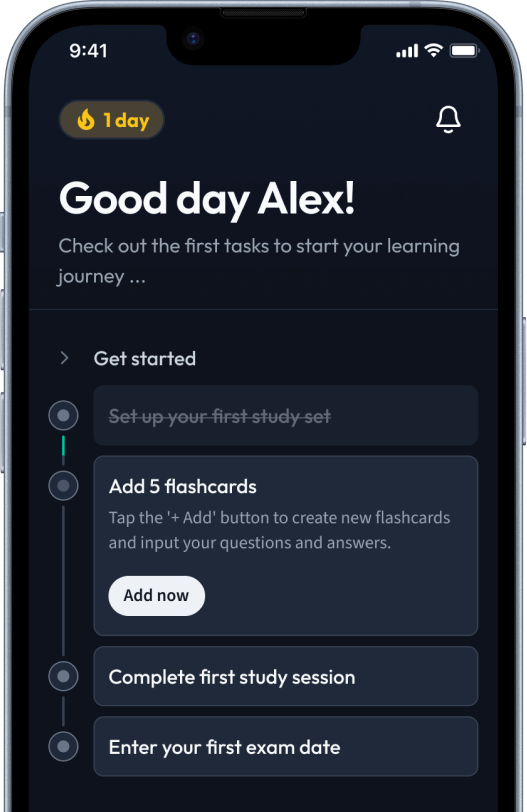
StudySmarter: Study help & AI tools
4.5 • +22k Ratings
More than 22 Million Downloads
Free
Delve into the fascinating world of Biology with a comprehensive exploration of vaccines. Unravel the layers of this crucial medical breakthrough, from understanding its basic concept to dissecting its multilayered connection with our cells. Historically significant vaccines will be spotlighted, along with diverse types applied in modern medical practices. The discussion goes beyond the biological, examining the ethical dimensions and societal implications attached to vaccine use. Stay informed, gain knowledge and explore the role of vaccines in building a society resilient to disease.


Lerne mit deinen Freunden und bleibe auf dem richtigen Kurs mit deinen persönlichen Lernstatistiken
Jetzt kostenlos anmeldenDelve into the fascinating world of Biology with a comprehensive exploration of vaccines. Unravel the layers of this crucial medical breakthrough, from understanding its basic concept to dissecting its multilayered connection with our cells. Historically significant vaccines will be spotlighted, along with diverse types applied in modern medical practices. The discussion goes beyond the biological, examining the ethical dimensions and societal implications attached to vaccine use. Stay informed, gain knowledge and explore the role of vaccines in building a society resilient to disease.
In the wide field of biology, vaccines play a prominent role in preventive healthcare. They are biological preparations providing active acquired immunity against a certain disease. They typically contain an agent resembling a microorganism causing the disease. Through this process, vaccines prepare your body to fight off potential infections.
Since their inception, vaccines have saved countless lives and have been instrumental in eradicating diseases like smallpox globally.
Vaccines are agents that resemble infectious organisms. They stimulate the immune system to recognize these foreign agents and build a defence mechanism against them. When a vaccinated individual encounters the actual disease agent, their immune system is prepared to respond more effectively.
Let's take a trip down memory lane to understand the historical relevance of vaccines.
The smallpox vaccine, introduced by Edward Jenner in 1796, was the first vaccine to be developed. Jenner's breakthrough was based on an observation that milkmaids who contracted cowpox did not show signs of smallpox after exposure. Variolation, a method of the smallpox vaccine, was practiced until the mid-1800s when Jenner's method became standard.
The different types of vaccines have unique characteristics that make them useful against certain types of diseases.
| Live-attenuated vaccines | Used against diseases like measles, mumps, and rubella |
| Inactivated vaccines | Used for illnesses such as flu and polio |
| Subunit vaccines | Effective against diseases like Hepatitis B and HPV |
| Conjugate vaccines | Used for diseases like Haemophilus influenza type b |
Some vaccines for common diseases have become standard in medical practice, protecting individuals from these conditions throughout their lives.
Understanding how vaccines work at the cellular level can help shed light on their vital role in preventing diseases. When a vaccine enters your body, it stimulates an immune response, which involves various cells in your immune system. The result of this process extends far beyond just immediate protection against a specific pathogen; it leads to long-term immunity. Let's dive deeper into this mechanism.
The primary purpose of a vaccine is to educate your immune system about a specific pathogen, enabling it to recognise, respond to, and remember the invader.
Immunity is the body's ability to resist an infectious disease, usually through the presence of antibodies. Vaccination is a way to induce immunity artificially. The key players in this induction include cells such as B lymphocytes and T lymphocytes.
There are several stages to the immune response initiated by a vaccine. These include:
In other words, vaccines harness the immune system's power of memory.
B lymphocytes and T lymphocytes, or simply B cells and T cells, play a crucial role in the immune response.
B cells are a type of white blood cell that can recognise the antigens of pathogens and produce antibodies. Antibodies can block pathogens from invading cells and signal other immune cells to attack the pathogens.
T cells, another type of white blood cell, come in two main types: helper T cells, which coordinate immune responses, and cytotoxic T cells, which kill infected cells directly.
Together, these cells are cornerstones in creating a robust, efficient, and long-lasting immune response.
Despite their considerable benefits, vaccines also have some limitations and can encounter problems, mainly regarding their storage, handling, and delivery. Vaccine efficacy can be diminished with poor handling methods and inappropriate storage conditions.
Key limitations and issues often encountered with vaccines include:
The 'cold chain' refers to a temperature-controlled supply chain, ensuring that vaccines are stored and transported within the safe temperature range from the point of manufacture until administration.
Maintaining the cold chain is critical to the stability and effectiveness of vaccines. Temperature deviations can lead to reduced vaccine potency, resulting in inadequate immune responses in recipients.
Proper vaccine management is crucial, considering the following points:
Recent innovations, such as the use of thermostable vaccines and solar refrigeration, are expanding the possibilities of vaccination in remote and resource-limited settings. It signifies the continual advancement and evolution in the field, overcoming the limitations of vaccine storage and handling.
Vaccines, while primarily a biological tool, deeply intersect with the realms of sociology and ethics. They form an integral part of public health measures and bring to light the concept of herd immunity. However, their use sometimes sparks ethical debates. Understanding these facets is crucial to fully grasp the role vaccines play in society.
Herd immunity, also referred to as community immunity, is a protective mechanism that occurs when a large proportion of a community becomes immune to a specific infection, thus providing indirect protection to those who are not immune.
Vaccines have been instrumental in achieving herd immunity against various diseases. This principle underpins the strategy of mass vaccination campaigns, where the aim is not only to protect individuals but also to interrupt the transmission of disease in a population.
The level of vaccination coverage required to achieve herd immunity varies for different diseases. It depends on several factors, including the efficacy of the vaccine, the duration of the immunity it provides, and the characteristics of the disease in question. For instance:\[R_{0}\], is a key epidemiological metric indicating the number of additional infections that one case of disease can cause in a fully susceptible population. The higher the \[R_{0}\], the more people need to be immune to achieve herd immunity.
The core points regarding herd immunity are:
History is replete with instances when herd immunity has been achieved through vaccination. One such example is the eradication of smallpox. The World Health Organization launched an intensified plan in 1967 to eradicate smallpox. By maintaining high levels of population immunity through vaccination over a decade, the transmission of the virus was halted. Smallpox was formally declared eradicated in 1980, showcasing the power of vaccination and herd immunity.
Vaccination should ideally be a straightforward issue, considering its benefits to individual and public health. However, it often finds itself in a complex web of ethical discussions. Issues such as vaccine accessibility, mandating vaccination, and informed consent are key areas of contention and are pivotal in shaping the vaccination landscape.
Key ethical considerations often revolving around vaccines include:
Public Health Ethics refers to the principles and values that guide the practice of public health. It often involves balancing individual rights and liberties against the population's health needs.
Vaccines stand at the crossroads of individual rights and public safety. The role vaccines play in preventing and controlling disease outbreaks makes them a vital public health tool. Their impact goes beyond individual health benefits, contributing significantly to community health welfare.
However, the introduction of mandatory vaccination policies sometimes sparks resistance. Public health ethics thus come into play and often guide such decision-making processes. They ensure that the collective benefits of vaccination do not override individuals' right to autonomy, amongst other things.
Addressing this challenge requires considerable efforts in public health communication and community engagement. Clear, transparent, and empathetic communication can address vaccine hesitancy effectively and uphold the central public health ethics tenet - enabling individuals to lead healthier lives.
What is inside a vaccine?
Inside a vaccine is the specific antigen of the pathogen being vaccinated against. Vaccines contain either a weakened or dead version of these pathogens to allow the immune response to easily overcome the infection and prevent the vaccinated individual from developing symptoms of the disease.
How do vaccines work?
Vaccines work by triggering the primary immune response. When the antigen from the vaccine is detected in the body T cells are stimulated. Helper T cells stimulate B cells which secrete specific antibodies against the pathogen. Memory cells are also produced. These provide long-term immunity because they quickly secrete specific antibodies and destroy any of the same pathogens that enter the body in the future.
What type of immunity does vaccination produce?
Vaccination is an example of artificial active immunity. It is artificial because antigens are artificially introduced by humans rather than naturally through infection. It is active because the immune response develops antibodies using B cells, rather than antibodies being directly introduced into the body, which is passive immunity.
What are the two different types of vaccines?
Live attenuated and inactivated are the two different types of vaccines. Live attenuated vaccines contain a weakened or damaged version of a pathogen. Inactivated vaccines contain a dead version of the pathogen or a subunit of the pathogen, such as proteins.
What is an example of a vaccine?
MMR, the measles, mumps and rubella vaccine OR the HPV vaccine
What is herd immunity?
Herd immunity is when the majority of the population are vaccinated against a disease, resulting in a break in a diseases' transmission. This prevents those who are unvaccinated from coming into contact with the pathogen and becoming ill.
Already have an account? Log in
Open in AppThe first learning app that truly has everything you need to ace your exams in one place
Sign up to highlight and take notes. It’s 100% free.
Save explanations to your personalised space and access them anytime, anywhere!
Sign up with Email Sign up with AppleBy signing up, you agree to the Terms and Conditions and the Privacy Policy of StudySmarter.
Already have an account? Log in