
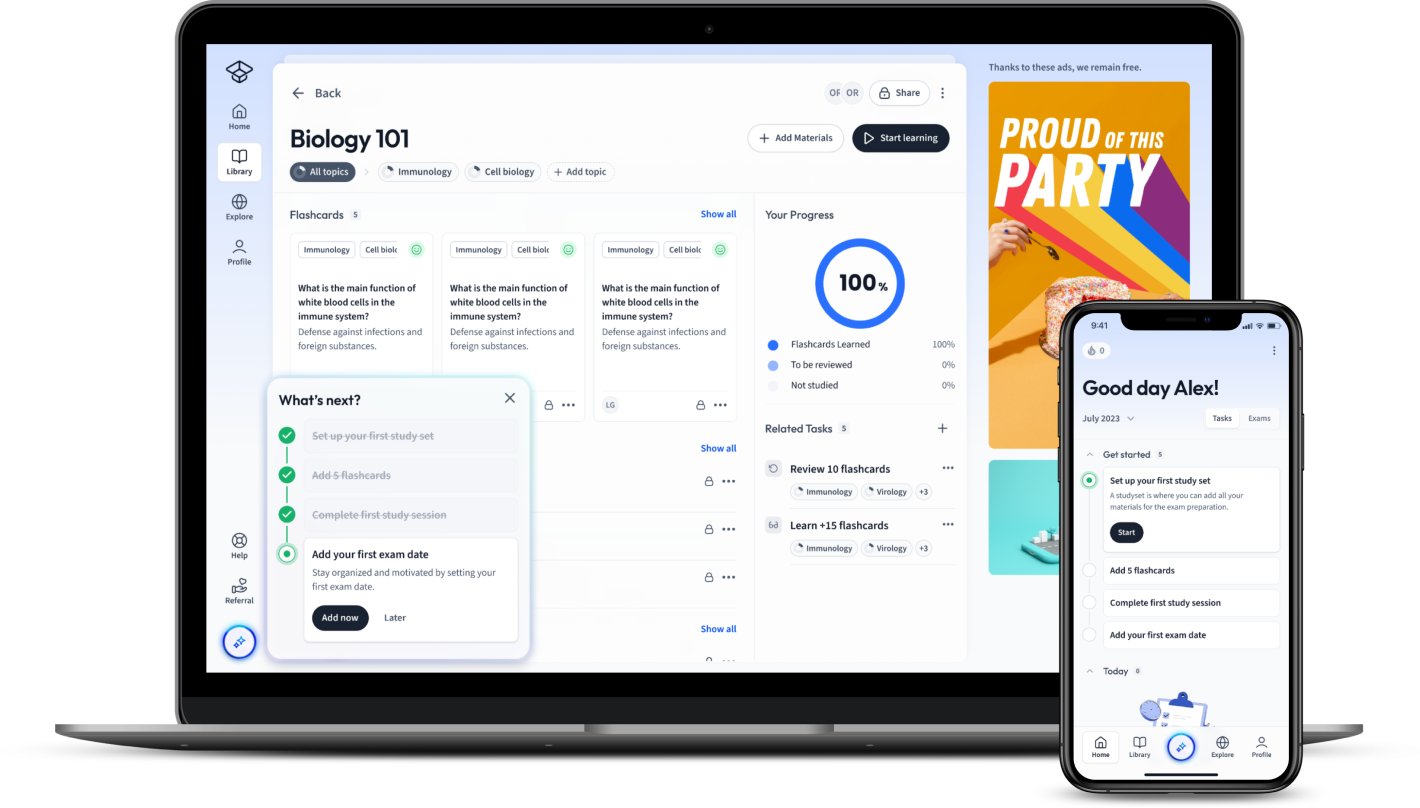
StudySmarter: Study help & AI tools
4.5 • +22k Ratings
More than 22 Million Downloads
Free
Dive into the expansive universe of microbiology with an in-depth exploration of antifungal, its significance, types, uses, and potential side effects. Discover the essence and importance of antifungal in microbiology, disentangle common misconceptions, and distinguish between different antifungal types. Learn about the therapeutic applications and risks associated with antifungal use, and the essential role antifungal medication plays in treating communicable diseases. Empower your knowledge and understanding, echoing the intricacies of this powerful tool in the fight against fungal diseases.


Lerne mit deinen Freunden und bleibe auf dem richtigen Kurs mit deinen persönlichen Lernstatistiken
Jetzt kostenlos anmeldenDive into the expansive universe of microbiology with an in-depth exploration of antifungal, its significance, types, uses, and potential side effects. Discover the essence and importance of antifungal in microbiology, disentangle common misconceptions, and distinguish between different antifungal types. Learn about the therapeutic applications and risks associated with antifungal use, and the essential role antifungal medication plays in treating communicable diseases. Empower your knowledge and understanding, echoing the intricacies of this powerful tool in the fight against fungal diseases.
When delving into the field of microbiology, the term "antifungal" undoubtedly surfaces frequently. This is because combating fungal infections is an integral part in safeguarding human health. Understanding the basics of antifungal medicines is equally critical for both aspiring and established microbiologists.
Antifungal is a term used to describe a class of medications used to treat fungi or fungal infections. Examples of these fungi are yeasts and molds, which can cause infections in various parts of the body.
Antifungal medications work by interfering with the cellular structures of the fungi or preventing their growth and reproduction.
These medicines can be classified into different types, including:
Each type targets a specific aspect of the fungal cell. For instance, \(Azoles\) inhibit the production of a compound called ergosterol which forms the cellular membrane of the fungus.
The structure of antifungal medications is crucial to understand how they function. For instance, the Azole class of antifungals, which includes drugs like clotrimazole and fluconazole, contains a five-membered heterocyclic ring. This ring is responsible for inhibiting the enzyme lanosterol 14 alpha-demethylase which is necessary for ergosterol production.
Antifungal agents are highly significant in microbiology for various reasons. They are crucial in controlling fungal growth, not just in the medical field, but also in environments such as industries and agriculture. For the sake of effective treatment, microbiology labs carry out susceptibility testing for fungi. This is a process which involves exposing fungi in the lab to various antifungal agents to gauge how sensitive or resistant they are to these drugs. Thus, it helps in deciding the most effective antifungal treatment for an infection.
It's also interesting that antifungal agents have been derived from various sources over the years, including other fungi and bacteria. This ties back into how interconnected different aspects of microbiology can be.
For example, penicillin, a common antibiotic, was derived from the Penicillium fungi. Similarly, bacteria from the Streptomyces species led to the discovery of both nystatin and amphotericin B, which are antifungal polyenes.
There are various misconceptions regarding antifungal usage, more so due to a lack of understanding of these drugs. These misbeliefs can often cause complications when treating infections if not addressed properly.
The first common misconception is, 'The more antifungal medicine one takes, the quicker the infection will clear.' The reality, however, is that antifungal medications need to be taken in moderation and as prescribed by a healthcare professional. Otherwise, it can lead to drug resistance among the fungi.
Another misunderstanding is that 'Antifungal creams alone are enough to treat all fungal infections.' This belief is erroneous since the type of fungal infection and its severity dictate the treatment method, and creams might not be suitable for all types of infections.
For instance, systemic or invasive fungal infections, like candidemia, which spread throughout the body often require intravenous antifungal medications such as fluconazole, Amphotericin B, or caspofungin.
A third common belief is that 'Antifungal and antibacterial medications are the same.' This misconception can prove to be harmful as bacteria and fungi differ greatly, and hence, require different kinds of treatments. Antifungal medications target specific components of the fungal cell, while antibacterial medications are effective against bacteria.
Antifungal medicines come in a variety of forms, each targeting specific types of fungi or parts of the fungal cell. These diverse types of antifungal lead to differences in their effect and application. Knowing these distinctions is crucial in microbiology.
Antifungal medications can primarily be categorised into four types: Azoles, Echinocandins, Polyenes, and Allamines.
It is rather important to note that the effectiveness of these medications can vary based on the specific type of fungi and the patient's health condition.
Ergosterol: a component of fungal cell membranes, providing fluidity and integrity, much like cholesterol in animal cells.
Understanding the key differences between the various types of antifungal medicines is crucial for effective treatment. Their differences mainly arise due to their structure and their mechanism of action.
The following table provides an overview of the differentiating factors between these classes:
| Type | Main Function | Examples |
| Azoles | Interferes with ergosterol synthesis | Fluconazole, Ketoconazole |
| Echinocandins | Inhibits synthesis of the fungal cell wall | Caspofungin, Micafungin |
| Polyenes | Binds to ergosterol to form pores | Amphotericin B |
| Allamies | Hinders production of squalene epoxidase | Terbinafine |
This categorization can help healthcare professionals determine the ideal course of treatment for patients with fungal infections. It's important to remember that each class has distinct properties and side-effects. For instance, while azole antifungals tend to have fewer side effects and can be taken orally, polyene antifungals might cause kidney damage and hence are used in severe cases only.
Additionally, antimicrobial resistance is an emerging challenge in the treatment of fungal infections. A fungus can develop resistance to a specific type of antifungal drug, making it less effective. This reaffirms the need for an in-depth understanding of the different types of antifungal medications to ensure the administration of the most effective treatment.
Going beyond the realm of microbiology, the use of antifungal medications spills over into various fields such as healthcare, agriculture, and industries. The importance and potential of antifungal agents are emphasised by their wide-ranging applications in treating communicable diseases and other therapeutic uses.
Antifungal agents serve a multitude of purposes catering to a variety of scenarios. These primarily revolve around the treatment and management of fungal infections. However, what's intriguing is how these uses span different domains, industries and application areas beyond health and medicine.
Within the healthcare sector, antifungal medications are extensively used for treating a spectrum of fungal infections ranging from minor skin infections to life-threatening systemic ones. Take ringworm or athlete's foot, for example — these skin infections are normally treated by over-the-counter topical creams that contain antifungal substances like clotrimazole or miconazole.
Apart from healthcare, antifungal compounds occupy a significant place in agriculture. They are utilised to control and prevent the growth of fungi on crops, which is crucial in increasing crop yield and protecting food supplies. Specific antifungal agents, such as copper compounds or sulfur, are often used in fungicides to prevent the outbreak of plant diseases caused by fungi.
In industrial settings, antifungal substances are used to treat mould growth. Be it in the paint industry, wood preservatives or even in the making of detergents, antifungals help in warding off fungal growth that may cause spoilage or deterioration.
For instance, (Z)-2-decenoic acid, a fatty acid derived from the fungus Macrophomina phaseolina, has been evaluated for its antifungal activity and potential use as a biofungicide in agricultural settings.
Antifungal medications embody a critical role in managing communicable diseases caused by fungi. What sets fungal infections apart from bacterial or viral ones, is their propensity to occur due to opportunistic fungi. These are types of fungi which ordinarily wouldn't cause an infection but can do so in individuals with a compromised immune system.
Fungal diseases such as Aspergillosis, Candidiasis, Cryptococcosis and Histoplasmosis are relatively common and can become serious without effective antifungal treatment. Just like how antivirals are used against viral diseases or antibiotics against bacterial ones, antifungal medications are leveraged against such fungal diseases. Depending on the severity and nature of the infection, healthcare professionals prescribe either topical or oral antifungals, or in severe cases, intravenous antifungal drugs.
Antifungal prophylaxis, the preventive administration of antifungal agents, is also practiced extensively in patients at high risk of developing fungal infections. This can include patients undergoing surgeries, individuals with HIV/AIDS, or those receiving chemotherapy. It reduces the chances of a potential fungal infection from developing and becoming a health risk.
Opportunistic Fungi:: Types of fungi which ordinarily wouldn't cause an infection but can do so in individuals with a compromised immune system.
Moving closer to a patient-level view, antifungal medications have an impressive array of therapeutic applications in medicine. Their use extends beyond just curative treatments and delves into preventive and maintenance therapy for an array of fungal infections.
Superficial fungal infections, those that affect the skin, hair and nails, are often effectively treated using topical antifungal medications. These include creams, lotions, or gels that contain antifungal compounds and can kill fungi or prevent their growth.
Systemic infections are those that affect internal organs and can pose serious health threats if left untreated. Here, the use of systemic antifungal agents, which are often administered orally or intravenously, becomes necessary.
Forging ahead, a noteworthy domain of antifungal therapy revolves around drug combinations. As the battle with resistant strains of fungi continues, combining various types of antifungal medications improves the chances of successful treatment. This is particularly useful in treating complex and severe systemic infections. An example can be seen in the combined usage of Amphotericin B and Flucytosine in the initial phase of the treatment for cryptococcal meningitis — a potentially deadly fungal infection.
Lastly, although commonplace, self-medication with over-the-counter antifungal medications is yet another therapeutic application of antifungal agents. These are normally used for uncomplicated skin or vaginal fungal infections.
To conclude, the applications of antifungal agents are far-reaching and continue to grow, as scientists harness their power in diverse and innovative ways.
Antifungal medications, like all pharmaceutical treatments, can cause side effects. Although often effective in combating fungal infections, it's critical to recognise the possible adverse reactions associated with these medications. These side effects can range in severity from minor irritations to significant health complications. Navigating these potential drawbacks is integral to ensuring the safety and well-being of those undergoing such treatments.
When learning about antifungal side effects, it is important to understand that they can occur differently based on various factors. Whether these side effects present themselves depends on the type of antifungal medication used, the individual characteristics of the patient, duration of use, and the dosage.
The most common set of side effects stem from azole antifungal medications which include Fluconazole, Itraconazole, and Ketoconazole, among others. Patients may suffer symptoms such as:
In rare, more serious cases, azoles may cause more severe side effects including hepatitis and severe skin reactions. Polyene antifungals, such as Amphotericin B, may lead to side effects like:
Of particular note here is Amphotericin B, renowned for its tough side effects. It also leads to something informalily known as 'shake and bake' phenomenon where patients may suffer severe chills and high temperature following its administration.
Allylamines like Terbinafine, cause gastrointestinal side effects primarily, as well as headaches and rash. Lastly, echinocandins are generally more tolerable, but may still cause nausea, diarrhoea and fever.
It should be noted that allergic reactions to antifungal medications may also occur, though they are quite rare. These can lead to severe issues like difficulty breathing and swelling in the face or throat.
'Shake and Bake' Phenomenon: A term for the reaction often witnessed in patients after the administration of Amphotericin B, characterised by severe chills and high body temperature.
Side effects represent one of the fundamental challenges in treating fungal infections with antifungal agents. They can impact the patient's quality of life, adherence to the treatment and in rare cases, their overall health outcomes.
Among the spectrum of side effects, some are only mild and temporary, clearing up on their own. These include brief digestive discomfort or mild skin rash. However, other side effects demand immediate attention. These may potentially be life-threatening conditions such as severe skin reactions, liver or kidney damage, or allergic reactions.
While the rate and severity of side effects can depend on various patient factors, understanding the mechanisms of how these antifungals work can create a broader picture. Antifungal agents target the fungal cells and their growth mechanism which, unfortunately, sometimes adversely affects human cells too.
Furthermore, it's vital to bear in mind that self-medication and not sticking to a medication regimen can lead to irresponsible use, thereby increasing the risk of side effects. In particular, the inappropriate usage of antifungal medications may lead to 'antifungal resistance', which occurs when the fungi being treated by the medication adapt to its effects, making the drugs less effective. This undesirable scenario not only makes treatment difficult but also increases the possibility and intensity of unwanted side effects.
Antifungal Resistance: When fungi adapt to the effects of antifungal medications making the drugs less effective, hence making treatments more difficult.
Adverse side effects often hinder patient adherence to antifungal medication. A departure from the recommended treatment program may lead to treatment failure or aid the development of drug-resistant strains of fungi. Therefore, treatment strategies must strike a balance between the effectiveness of the antifungal medication and its potential side effects.
To that end, healthcare professionals must endeavour to provide healthcare education that underlines the importance of accurately following the antifungal treatment regimen whilst also detailing the possible side effects. Both these aspects in harmony will aid in maximizing the benefits of treatment and minimizing the potential risks.
Antifungal medications play a pivotal role in combatting various forms of invasive and superficial fungal infections. Capable of halting the growth of fungi in the human body, these therapeutics function to alleviate symptoms, treat the root infection and prevent potential relapses. Ranging from over-the-counter topical creams to systemic medications, the role of antifungal treatments is wide and varies based on the severity and type of fungal infection at hand.
The chief aim of antifungal medication is to incapacitate the capacity of the fungi to reproduce or thrive, thereby hindering further progression of the infection. Depending on the type and grade of infection, different classes of antifungal agents can be employed. These include azoles, polyenes, echinocandins, and allylamines, each of which targets a specific phase of the fungal cell life cycle or specific attribute of the cell makeup.
Antifungal medications can be administered via various routes – topical, oral, and intravenous. Topical applications, typically in the form of ointments or creams, are used for skin, nail or mucosal surface infections. Oral and intravenous treatments are usually enlisted to treat more severe or systemic fungal infections. It is crucial to note that each method of administration varies in terms of exposure to the systemic circulation and its subsequent effects or side effects.
Antifungal resistance, where the fungi adapt to the effects of the medication rendering it less effective, is a growing issue in the medical field. This phenomenon results from the overuse or misuse of antifungals and is a concern particularly in candida type infections. It serves as an urgent call for responsible medication usage and continued research into new antifungal agents and strategies.
Patients need to understand the importance of strict adherence to antifungal therapy, and the potential implications of non-compliance. This often includes the necessity of completing the entire course of therapy to prevent relapse or resistance development, even if symptoms have subsided.
When treating any fungal infection, healthcare providers will first identify the infecting fungus to determine the most suitable antifungal agent for treatment. A simple antifungal cream for minor skin infections such as athlete's foot or ringworm may suffice. But more serious infections like systemic candidiasis require strong systemic antifungal treatment.
Though antifungal medications can successfully treat many fungal infections, they do carry risks of side effects as well. The most common ones usually involve nausea, vomiting, abdominal pain, and diarrhoea with systemic treatments. On the other hand, topical treatments might cause skin irritation, burning sensation, or redness at the site of application. Some antifungals can also interfere with other medications the patient may be taking, causing adverse drug interactions.
Considering the potentially harmful side effects and drug-resistant risks of antifungal medication misuse, it is recommended to use such treatments only under the guidance of healthcare providers. Self-treatment with over-the-counter antifungal creams or pills may seem convenient, but it can lead to incorrect diagnosis and improper usage.
Fungal infections such as candidiasis, aspergillosis, and cryptococcosis significantly contribute to communicable diseases, especially among immune-compromised people including HIV/AIDS and cancer patients. Antifungal drugs play a critical role in reducing the morbidity and mortality associated with these infections.
The efficacy of antifungal treatments in communicable diseases is often highlighted by its ability to control and eliminate invading fungi in the body, stopping the spread of infection and helping the body recover. However, it should be noted that the success of such treatments depends heavily on early detection and initiation of therapy.
There is a growing concern about the rise of antifungal resistance among certain types of fungi, with candida species leading the list. This resistance has been linked to increased mortality rates, longer hospital stays, and higher healthcare costs. As such, antifungal stewardship programmes, that aim to control the use of antifungal agents to prevent resistance, are being implemented in many healthcare settings.
Antifungal treatment, when used appropriately and responsibly, can be a powerful tool in the battle against communicable fungal diseases. By understanding its proper use, side effects, and the risk of resistance, patients and healthcare providers alike can work together to optimise its benefits and minimise potential damage.
What is the role of antifungal agents in microbiology?
Antifungal agents control fungal growth, crucial not just in medicine, but also in industries and agriculture. They also aid in susceptibility testing for fungi, helping determine effective treatment methods. Some antifungal agents are derived from bacteria and other fungi, representing microbiology's interconnectedness.
What is the misconception about antifungal and antibacterial medications?
A common misconception is that antifungal and antibacterial medications are the same. They aren't because they target different organisms. Antifungal medications target specific components in fungal cells, while antibacterial drugs are effective against bacteria.
How do antifungal medications, particularly Azoles, work?
Antifungal medications interfere with fungal cellular structures or prevent their growth and reproduction. Specifically, Azoles inhibit the production of ergosterol, forming the fungal cell membrane, by blocking the enzyme lanosterol 14 alpha-demethylase needed for its production.
What are the four main categories of antifungal medications?
The four main categories of antifungal medications are Azoles, Echinocandins, Polyenes, and Allamines.
What role does ergosterol play in the functioning of antifungal medicines such as Azoles and Polyenes?
Ergosterol is a component of the fungal cell membrane. Azoles interfere with its synthesis causing the fungal cell to die, whereas Polyenes bind to ergosterol, forming pores and causing cell breakdown.
What is one key difference in the mechanism of action between Echinocandins and Allamines?
Echinocandins work by inhibiting the synthesis of the fungal cell wall, making the cells vulnerable to osmotic instability. Allamines, on the other hand, inhibit the enzyme squalene epoxidase, stopping ergosterol's biosynthesis.
Already have an account? Log in
Open in AppThe first learning app that truly has everything you need to ace your exams in one place
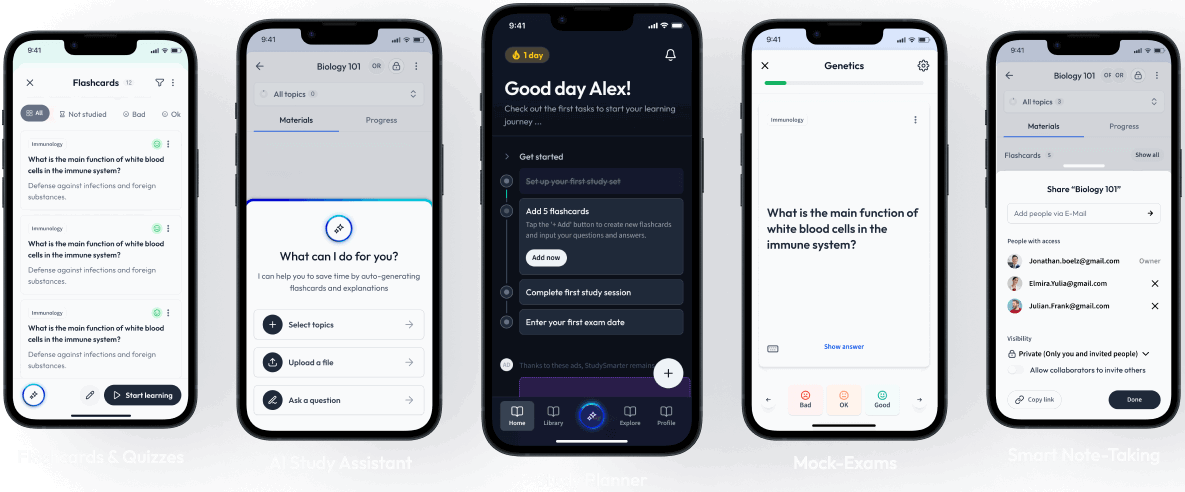
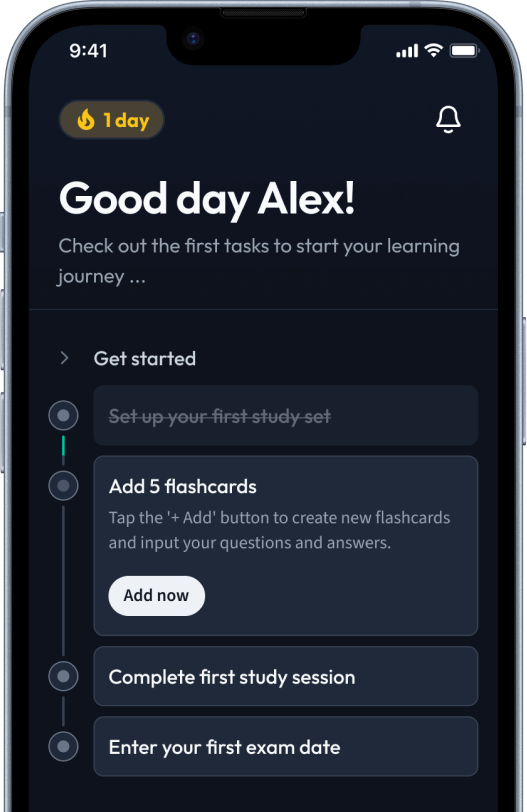
Sign up to highlight and take notes. It’s 100% free.
Save explanations to your personalised space and access them anytime, anywhere!
Sign up with Email Sign up with AppleBy signing up, you agree to the Terms and Conditions and the Privacy Policy of StudySmarter.
Already have an account? Log in