
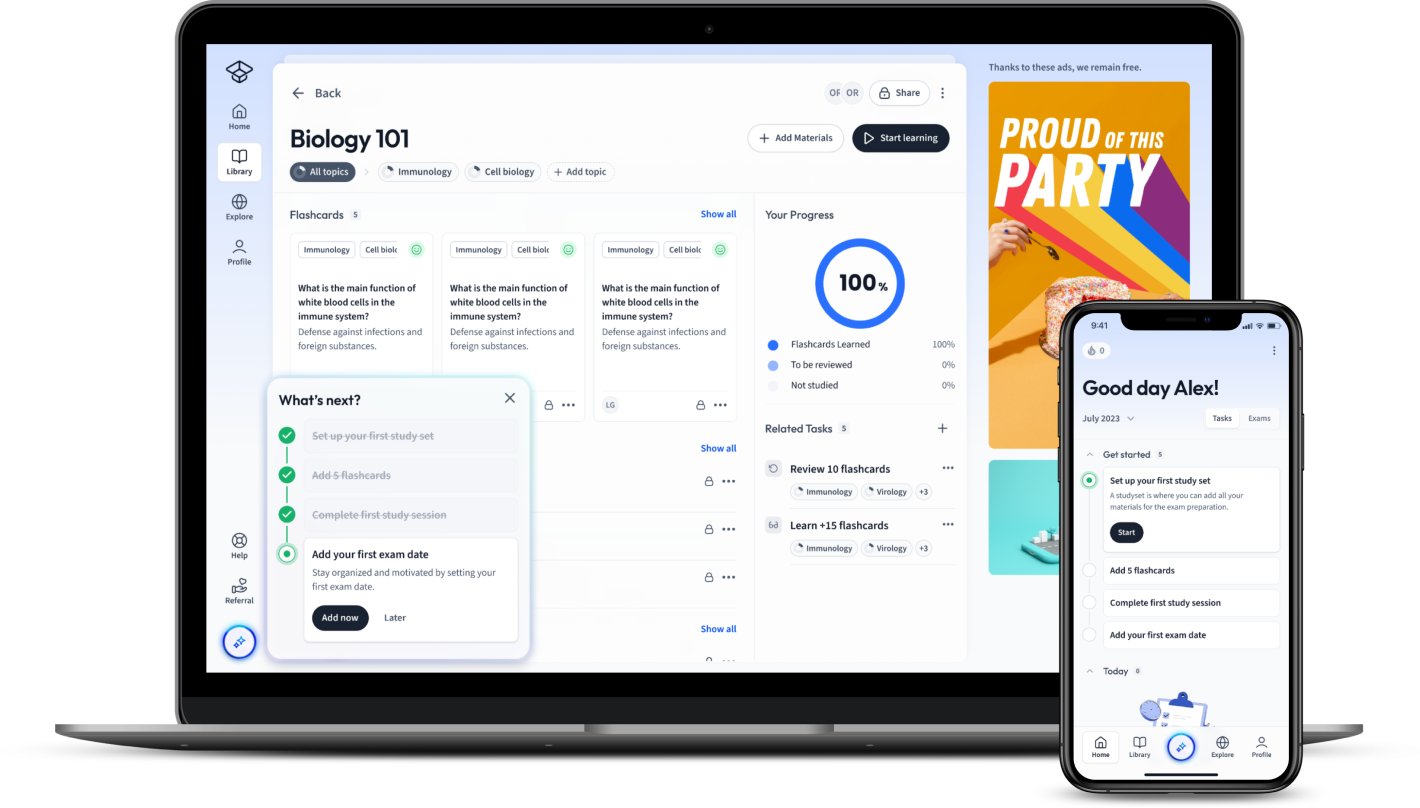
StudySmarter: Study help & AI tools
4.5 • +22k Ratings
More than 22 Million Downloads
Free
Delve into the fascinating world of microbes with a comprehensive examination of pathogenicity in microbiology. Unearth the basic concepts and various types of pathogenicity, such as primary versus opportunistic and inherent versus acquired. Explore in-depth the significant role of pathogenicity factors in disease spread and microbial infections, and gain valuable insights into common pathogenicity mechanisms. Further, this comprehensive guide will shed light on the crucial determinants of pathogenicity and how it influences disease spread, severity, and prevention methods. Finally, understand the future of disease control in the context of minimising pathogenicity impact.


Lerne mit deinen Freunden und bleibe auf dem richtigen Kurs mit deinen persönlichen Lernstatistiken
Jetzt kostenlos anmeldenDelve into the fascinating world of microbes with a comprehensive examination of pathogenicity in microbiology. Unearth the basic concepts and various types of pathogenicity, such as primary versus opportunistic and inherent versus acquired. Explore in-depth the significant role of pathogenicity factors in disease spread and microbial infections, and gain valuable insights into common pathogenicity mechanisms. Further, this comprehensive guide will shed light on the crucial determinants of pathogenicity and how it influences disease spread, severity, and prevention methods. Finally, understand the future of disease control in the context of minimising pathogenicity impact.
In the field of microbiology, the term 'pathogenicity' carries immense significance. It denotes the ability of a microorganism, like bacteria, viruses, and others, to cause disease in a host. Meanings and types of pathogenicity differ depending on various factors. Delving profoundly into these concepts in the sections below.
To start with, let's unravel the basic concepts surrounding pathogenicity. In simple terms, pathogenicity is the capability of a microorganism to produce a disease. You need to understand that not all microbes are harmful; some live harmoniously within our bodies and even provide benefits. Only a small fraction of microbes are pathogenic, demonstrating the ability to invade the host's body, dodge the immune system and ultimately cause disease.
Pathogenicity is the capability of a microorganism to produce a disease.
Next, let's talk about virulence, a term that often comes hand in hand with pathogenicity. While pathogenicity refers to the ability to cause disease, virulence refers to the degree or severity of the disease. Microbes with high virulence cause severe diseases, while those with low virulence may not cause illness or result in very mild symptoms.
Virulence is a facet of pathogenicity; it's not just about whether a microbe can cause disease but how severe that disease can be.
The concept of pathogenicity isn't one-dimensional. When you dive deeper into microbiology, you'll find there are different types of pathogenicity - primary, opportunistic, inherent, and acquired. Understanding these variations can enhance your grasp of how different microbes interact with their hosts and lead to disease.
Primary Pathogens and Opportunistic Pathogens are two groups that you'll frequently encounter in microbiology. They significantly differ in how and when they cause disease.
Assume someone with a compromised immune system due to disease or medication. In this situation, common harmless bacteria in the gut might become opportunistic pathogens if they manage to reach the bloodstream, triggering a potentially life-threatening infection.
The categorisation of pathogenicity doesn't stop there. Another way to distinguish pathogenic bacteria is based on whether the pathogenic character is inherent or acquired.
| Inherent Pathogenicity | These are organisms that are naturally pathogenic. They pose a threat because of the virulence factors they inherently possess. |
| Acquired Pathogenicity | These organisms usually become pathogenic after acquiring new genes, often through horizontal gene transfer from other bacteria. Once they acquire these genes, they can potentially cause disease. |
Transposition or horizontal gene transfer is an interesting aspect of microbiology. This phenomenon allows bacteria to share genes, spreading beneficial traits - like antibiotic resistance or pathogenicity - within a population.
In the battle against disease, understanding how microbes become pathogenic - either inherently or through gene acquisition - is crucial. It helps scientists devise strategies to prevent and treat diseases.
Now that you've gathered an understanding of pathogenicity and its various types, it's time to dive deeper and explore the specific factors that contribute to microbes' ability to cause disease. These pathogenicity factors play significant roles in disease progression and microbial infection management.
The success of a microbe in causing disease lies in its capacity to survive and proliferate in the host's body, and the elements that enable this are known as pathogenicity factors.
Pathogenicity factors are the strategies and properties a microbe uses to invade, evade the host's immune response, reproduce and cause disease. These factors are crucial to understand because they help predict how microbial infections spread and how severe they can become.
Here is a list of some prominent pathogenicity factors:
Whether a microbial infection will occur and its ultimate severity largely depends on pathogenicity factors. These factors need to be understood as they present promising targets for treatment strategies. You will find that some antibiotics and vaccines focus on pathogenicity factors. For example, an antibiotic may inhibit toxin production, or a vaccine might provoke an immune response against a bacterium's adhesive structures, nullifying its ability to invade host cells.
Addressing pathogenicity factors in treatment has the added benefit of reducing the pressure of selection for antibiotic resistance. If a treatment targets something like toxin production rather than bacterial growth, bacteria will less likely develop the resistance since survival doesn’t depend on resisting the treatment.
Successful pathogens have to defy the host's defences to establish an infection, representing a significant pathogenicity factor. Bacteria have developed an array of mechanisms to resist these defences and ensure their survival.
Sometimes, bacteria protect themselves by neutralising the host’s weapons. For example, Staphylococcus aureus produces an enzyme known as beta-lactamase that can deactivate beta-lactam antibiotics, including widely-used antibiotics like penicillin, allowing it to resist these drugs and survive.
Another method is to hide from or confuse the host's immune system. Some bacteria encapsulate themselves with layers of polysaccharides, making it harder for the host immune cells to recognise or effectively destroy them.
The capability to spread within a host or between hosts is another major pathogenicity factor. Microbes have evolved numerous strategies to ensure their propagation, further contributing to their pathogenicity.
Inside the host, microbes can spread from the initial infection site to other areas. For instance, bacteria can move by following the natural pathways within the body, like the bloodstream or the lymphatic system. Moreover, they can use specific enzymes to "dig" pathways through tissues.
Between hosts, microbes rely on a multitude of transmission routes, including airborne droplets, physical contact, or the ingestion of contaminated food and water. These transmission routes are crucial for the microbe to continue its lifecycle and cause new infections.
In COVID-19, the SARS-CoV-2 virus spreads mainly through airborne droplets when people talk, cough, or sneeze. Viruses in these droplets can be inhaled into the lungs, initiating an infection.
The instance of an infection is likely a well-orchestrated scheme of events, governed by a set of strategic mechanisms known as pathogenicity mechanisms. These mechanisms are the steps and processes that pathogens use to invade, evade, replicate and eventually cause disease in the host.
To genuinely comprehend how infections burgeon and progress, you should appreciate the disease cycle's complexity in its entirety. Each stage of the disease cycle involves intricate mechanisms and strategies that fortify a pathogen's pathogenicity.
The disease cycle comprises the stages of pathogen entry, adhesion, invasion, replication, damage causation, and eventual exit. All these stages are overseen by unique pathogenicity mechanisms honed by microbial evolution.
A disease cycle denotes the continuous transmission of disease from the pathogen to the host and back, propagating through various stages like pathogen entry, adhesion, invasion, replication, damage, and eventual exit.
At the entry stage, pathogens leverage various mechanisms, such as adherence to host cells via adhesive structures like fimbraie, capsules or intrusions via breaches in the skin or mucosa.
Once inside, pathogens continue their invasion deeper into the tissues with the aid of enzymes and cytokines, disarming local host defences and paving the way for establishment and spread.
The capability of a pathogen to multiply or replicate within a host is paramount to its survival and ability to cause disease. Replication mechanisms are pathogenicity factors that enable rapid multiplication of pathogens within host cells.
Finally, the culmination point of the pathogenicity process is when damage is inflicted upon the host's tissues or systems by the pathogen. This damage can be direct, via cytotoxic elements, or indirect, driven by the host's inflammatory response.
Understanding the role and function of pathogenicity mechanisms in the disease cycle reinforces the essence of targeted antimicrobial therapy. Tailored interventions that inhibit these mechanisms impede disease progression and provide a more effective cure.
Shifting focus onto explicit pathogenicity mechanisms, you will uncover a wide array of tactics employed by microbes to cause disease. Predominantly, two vital mechanisms stand out - invasion and toxin production.
Consider a fort that must be breached for an enemy to invade: this is an apt metaphor for the invasion mechanism of pathogens. It not only relates to the physical breaching of host defences but also illustrates the strategies to evade the host's immune system.
Physical invasion involves the usage of adhesins, a sub-group of proteins that allow the pathogen to attach and establish an initial site of infection. Furthermore, microbes can release enzymes to break down tissue barriers, propagating further into the host's body.
| Adhesins | These proteins enable bacteria to stick to host cells, creating a foothold that can lead to infection. |
| Enzymes | These proteins can cause lysis of host cells, breakdown of physical barriers, or neutralisation of host defences, facilitating bacterial invasion. |
Besides physical invasion, pathogens also employ tactics to elude host immune defences. These mechanisms include antigenic variation, taking refuge inside host cells, or secreting 'fake' signals to confuse the host cells. Also, some can disable the host's immune cells directly, or even worse, turn them against the host itself.
The bacterium Listeria monocytogenes evades being killed by host immune cells by hiding inside these cells. While within a cell, it multiplies and eventually bursts the host cell, spreading to attack other cells.
Toxins are lethal substances that are produced and secreted by microorganisms, contributing immensely to their pathogenicity. On elaborating, you'll find two main types of toxins- endotoxins and exotoxins.
Endotoxins are part of the outer layer of the bacterial cell wall. When the bacteria die and split apart, these endotoxins are released and trigger massive inflammatory responses in the host. This can lead to fever, shock, or other harmful effects.
Exotoxins, on the other hand, are poisonous substances actively secreted by bacteria. They target specific cells in the host and jeopardise their function or cause cell death.
Toxin production is a potent pathogenicity mechanism that can drastically amplify the severity of the diseases caused by the pathogens. Indeed, some of the most perilous microbes known are so dangerous because of the toxins they produce.
In essence, toxins manipulate the regularity and harmony of the host's biological systems, leading to an array of symptoms and syndromes that signify a raging infection. Thorough understanding of bacterial toxins may foster novel therapeutic interventions, curbing the severity of resulting diseases.
In the realm of Microbiology, pathogenicity determinants play a crucial role in delineating the capacity of a microorganism to cause harm in a host. They are a constellation of genetic, biochemical, structural, and behavioural traits that contribute to an organism's potential to cause disease.
Communicable diseases, which spread from person to person or from an animal to a person, owe their spread to a plethora of pathogenicity determinants. Identifying these determinants is imperative for understanding disease progression and developing appropriate strategies for prevention and control.
From a genetic perspective, certain bacteria, viruses, and other microorganisms have specific genes that confer virulence, known as **virulence factors**. These genes typically encode proteins involved in adherence, invasion, evasion of host defences, and damage to the host. For instance, the fimH gene in E. coli bacteria encodes an adhesin, a protein involved in binding to host cells, which facilitates bacterial entry into the host.
| fimH gene | The fimH gene codes for a crucial protein in bacteria that facilitate their adherence to host cells. |
Moreover, the biochemical traits of microbes, such as their metabolism, nutrient requirements, and the toxins they produce, are vital pathogenicity determinants. For pathogens to survive and grow within a host, they must adapt to the environmental conditions within the host's body, such as varying pH, temperature, and nutrient availability. Metabolic adaptability, therefore, is a significant determinant of virulence.
The structural elements of a microbe also play a crucial role in pathogenicity. For instance, the thick, slimy 'capsule' present in certain bacteria provides a protective shield, helping the bacteria to evade the host's immune responses.
A microbial capsule is a polysaccharide layer that lies outside the cell wall and is associated with virulence. It protects cells from engulfment by eukaryotic cells, such as macrophages.
Every interaction between a pathogen and its host is shaped by a variety of pathogenicity determinants. These determinants do not function in isolation; rather, each determinant interacts in a complex manner with others to influence the pathogen's ability to infect and cause disease.
For instance, adhesion to host cells, often mediated by proteins encoded by virulence genes, is a crucial initial step in many infections. It enables the pathogen to resist the mechanical flushing forces found in many host environments such as airways, urinary tract, or the gut. Following adhesion, the pathogen may next evade the host’s immune system, using other virulence factors such as antigenic variation. Simultaneously, capability to utilize the host nutrients also favour survival and multiplication within the host. Finally, toxins released by the pathogens cause the actual damage to the host, manifesting as disease.
Antigenic variation is the mechanism by which an infectious organism alters its surface proteins to avoid being identified and attacked by the immune system of its host.
The expression of virulence genes significantly impacts the ability of a pathogen to cause disease. Simply possessing virulence genes isn't enough; the pathogen must also express these genes at the right time and in the right context during infection.
Many virulence genes are tightly regulated and are only expressed in conditions when they are advantageous to the pathogen. Furthermore, expression of some virulence factors might be inhibited until the pathogen has successfully infiltrated the host. For instance, toxin genes are not expressed until the pathogen is well established inside the host where nutrients are available for toxin production.
The expression of virulence genes can also be influenced by environmental signals, such as changes in temperature, pH, or nutrient availability. Fundamentally, the dynamic tuning of gene expression enables pathogens to adapt swiftly to various host environments, bolstering their survival, and increasing their potential to cause disease.
Natural environments and host habitats harbour a myriad of environmental factors that influence microbial pathogenicity. These external circumstances not only impact the survival and growth of a pathogen but can also influence their pathogenic potential. Some examples of environmental influences on pathogenicity include temperature, humidity, pH, and the stress conditions a microorganism is exposed to.
For instance, temperature often directly affects pathogen survival and the expression rate of pathogenicity determinants. Many pathogens are adapted to survive and propagate at body temperature, which is around 37 degrees Celsius for humans. However, temperature changes in the environment can hinder the growth and virulence of these pathogens. Some pathogens cope with such temperature shifts via the expression of heat-shock proteins that facilitate their survival and continued infection.
Furthermore, nutrient availability, often dependent upon the external environment, also shapes the pathogenic potential of microbes. Nutrient-rich conditions typically foster swift microbial growth and may enhance the expression of virulence factors, making microbes more pathogenic.
In essence, environmental factors constitute a significant part of pathogenicity determinants, dictating how well a pathogen survives, adapts, and inflicts harm in the host.
In the field of microbiology, pathogenicity is often used to describe the potential of a microorganism to cause disease. This facet is pivotal while studying communicable diseases, as it signifies the relationship between a pathogen and its host, particularly its capacity to inflict harm.
A detailed understanding of pathogenicity not only apprises us of a pathogen's ability to cause disease, but also reveals intricate information about its potential to spread and the severity of disease it might cause.
Let's consider transmission or the spread of disease first. Pathogenicity determinants such as certain virulence factors can increase a microbe's transmission rate. One example of this is the production of enzymes that degrade host tissues, allowing the pathogen to penetrate physical barriers and spread into new regions of the host organism.
Furthermore, certain pathogens have advanced mechanisms to survive harsh environmental conditions outside the host. These survival strategies, collectively representing an aspect of pathogenicity, enable the pathogens to disperse widely in the environment, enhancing their spread.
Now, let's examine how pathogenicity impacts the severity of a disease. The severity, or the pathogenic potential, is influenced by various factors such as:
A virulence factor is a molecule produced by a pathogen that increases its fitness by helping it to establish itself in the host, evade the host's defenses, or inflict damage to the host's tissues.
The comprehension of pathogenicity is profoundly impactful in strategising disease prevention tactics. For instance, recognising the strategies employed by pathogens to evade the host's immune system can provide valuable insights for developing strategies to enhance host immunity against these pathogens.
A classic example is the development of vaccines. Vaccines work by exposing the body to safe amounts of weakened or dead pathogens or toxins made by the pathogen, stimulating the body's immune system to recognise and destroy them. By understanding the specifics of a pathogen's virulence factors and the mechanisms they use to invade the host, vaccines can be created to prepare the immune system to fight these specific factors in real infections. In other words, immunisation leverages the knowledge of pathogenicity to train the immune system.
Moreover, the understanding of pathogenicity can guide the implementation of policies and guidelines for preventing the spread of communicable diseases. These guidelines can be designed to interrupt the pathogen's transmission pathways, thereby curbing disease spread.
As an illustration, in the case of airborne diseases, guidelines may include measures such as wearing masks, maintaining physical distancing, and ventilating indoor spaces. In the case of vector-borne diseases, measures may involve controlling the vector population, using insect repellents, or wearing protective clothing.
Knowledge of pathogenicity can inform the design of effective antimicrobial therapies by identifying potential targets. By studying the pathogenicity determinants, we can identify the critical mechanisms that are essential for a pathogen's survival, proliferation, or ability to cause disease.
Many current antibiotics and antimicrobial drugs work by specifically targeting and inhibiting these essential mechanisms. For example, antibiotics like penicillin target bacterial cell wall synthesis, a crucial mechanism for bacteria, thereby inhibiting their growth.
Also, with genomic technologies, we can genetically profile the pathogens, pinpoint their virulence genes, and design therapeutics to specifically target these genes. This approach marks the era of personalised medicine, with treatment strategies tailored to combat the specific pathogenic traits of an infecting pathogen.
As we look forward, the pivotal role that pathogenicity plays in understanding disease dynamics will continue to shape the future of disease control. With advancements in technologies, we are better equipped than ever to study the molecular determinants of pathogenicity in real time, at the individual pathogen level.
This will refine our knowledge of how individual genes in a pathogen contribute to pathogenicity, how they are regulated, and how they interact with the host and environmental factors. This knowledge will inform the design of targeted therapeutics and preventative measures.
Furthermore, studying pathogenicity provides a foundation for developing and advising public health policies aimed at minimising the impact of pathogenic microorganisms on humanity. These strategies, in conjunction with the increasing use of immunisation, surveillance, and prompt reporting of diseases, will shape the future of pathogen control and disease prevention.
What does the term 'pathogenicity' mean in the field of microbiology?
Pathogenicity refers to the capability of a microorganism, like bacteria, viruses, etc., to produce a disease. Not all microbes are harmful, a small fraction are pathogenic, demonstrating the ability to invade the host's body, dodge the immune system, and cause disease.
What is the difference between primary and opportunistic pathogens?
Primary pathogens can cause disease in a healthy host, bypassing the host's defenses to initiate an infection. Opportunistic pathogens, however, only cause disease in an immuno-compromised host, not harming their host unless the host's immunity is weakened.
How do inherent pathogenicity and acquired pathogenicity differ?
Inherent pathogenicity refers to organisms that are naturally pathogenic due to their inherent virulence factors. Acquired pathogenicity refers to organisms that become pathogenic after acquiring new genes, often through horizontal gene transfer from other bacteria.
What are pathogenicity factors?
Pathogenicity factors are the strategies and properties a microbe uses to invade, evade the host's immune response, reproduce and cause disease. These factors help predict the spread and severity of microbial infections.
What is the role of the pathogenicity factor adaptors?
Adaptors are structures that allow microbes to bind to and invade host cells. For instance, some bacteria have pilus or fimbriae that help them latch onto the host cells.
How does the ability to resist defences act as a pathogenicity factor?
Successful pathogens need to defy the host's defences to establish an infection. They might neutralize host’s weapons, like producing enzymes to deactivate antibiotics, or hide from or confuse the host's immune system.
Already have an account? Log in
Open in AppThe first learning app that truly has everything you need to ace your exams in one place
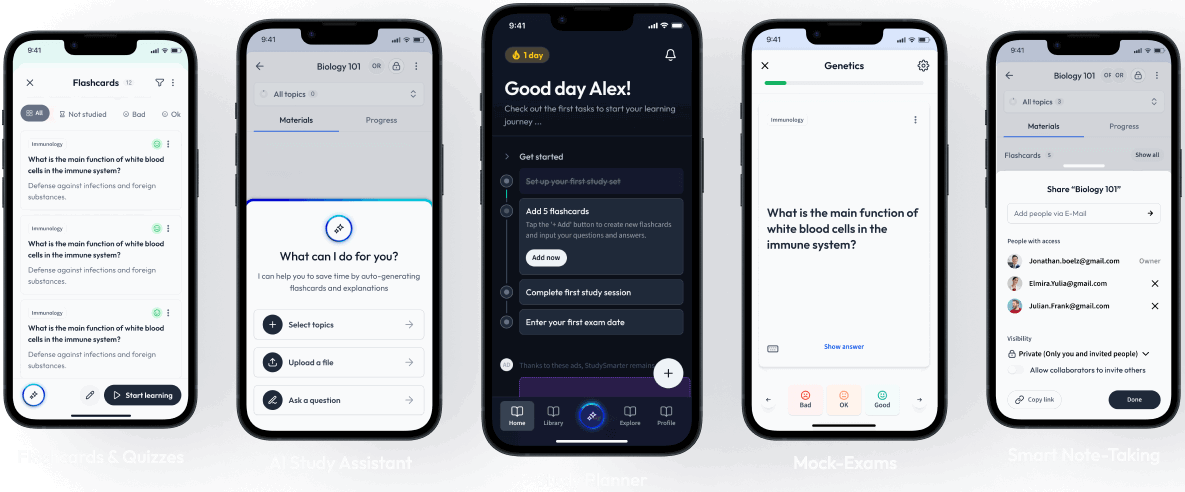
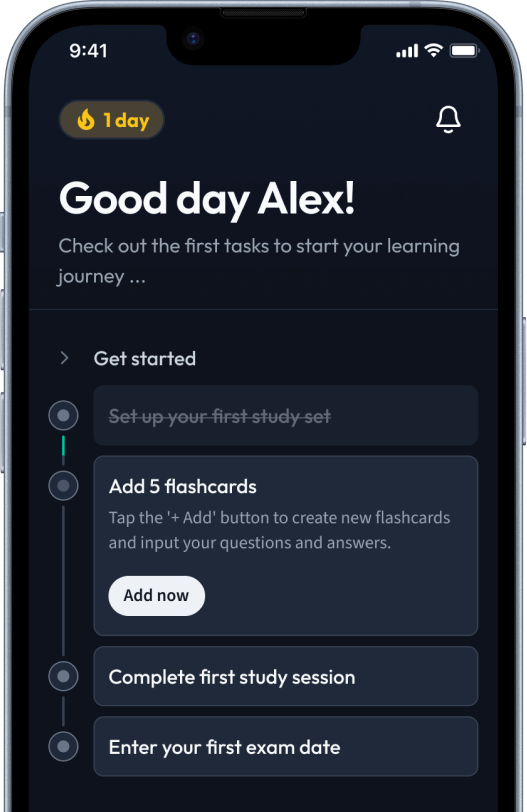
Sign up to highlight and take notes. It’s 100% free.
Save explanations to your personalised space and access them anytime, anywhere!
Sign up with Email Sign up with AppleBy signing up, you agree to the Terms and Conditions and the Privacy Policy of StudySmarter.
Already have an account? Log in