
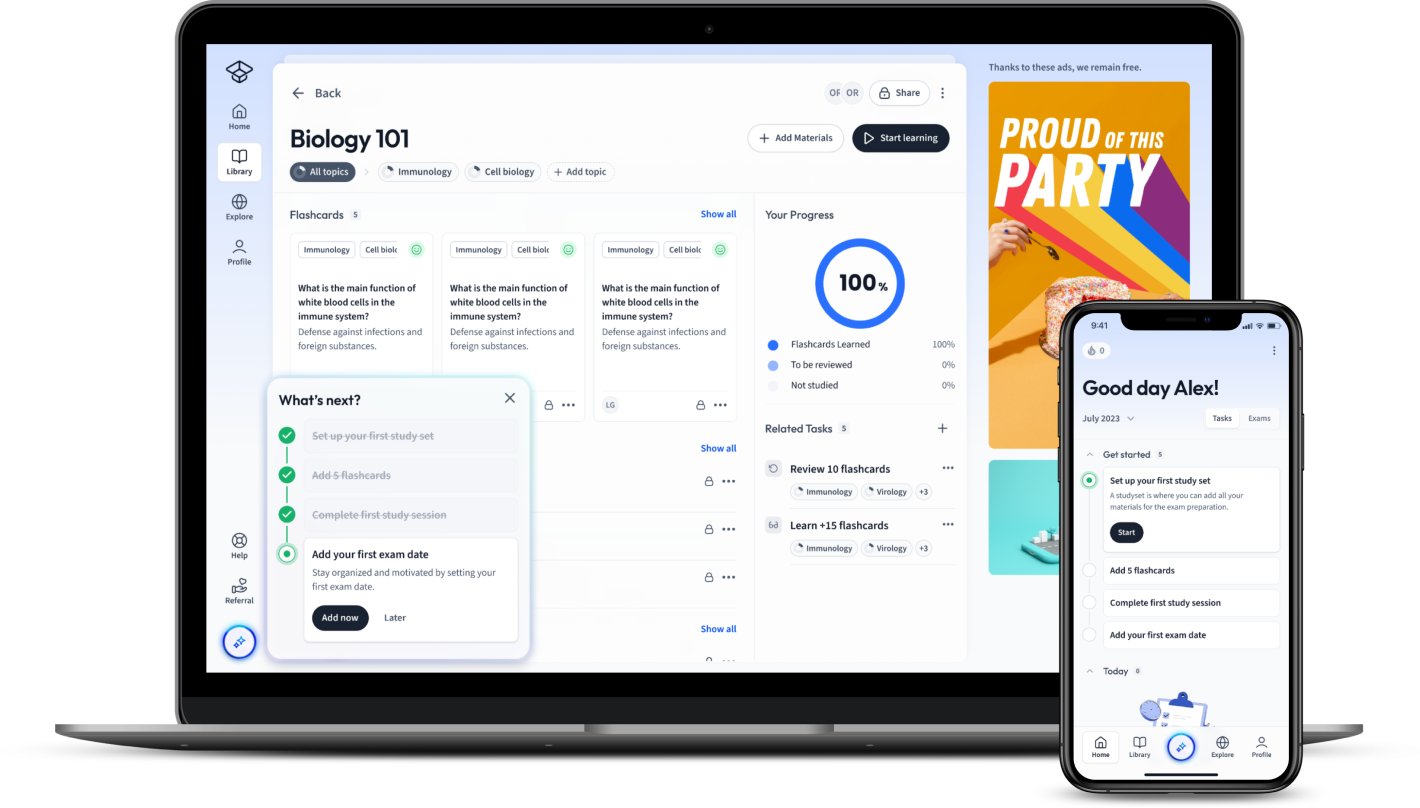
StudySmarter: Study help & AI tools
4.5 • +22k Ratings
More than 22 Million Downloads
Free
Delve into a comprehensive exploration of the various types of antibiotics, their diverse features, and unique modes of action. This incisive guide conveniently breaks down antibiotics into recognisable groups such as Penicillins, Cephalosporins, Macrolides, and more. Gain insights into how these antimicrobial substances interact with bacterial cells, their relevance to human health, and the specific medical conditions they treat. No matter if you're a student delving into the details of microbiology or a health professional seeking to refresh your knowledge, understanding the types of antibiotics and their applications plays a key role in achieving good health and combating formidable bacterial infections.


Lerne mit deinen Freunden und bleibe auf dem richtigen Kurs mit deinen persönlichen Lernstatistiken
Jetzt kostenlos anmeldenDelve into a comprehensive exploration of the various types of antibiotics, their diverse features, and unique modes of action. This incisive guide conveniently breaks down antibiotics into recognisable groups such as Penicillins, Cephalosporins, Macrolides, and more. Gain insights into how these antimicrobial substances interact with bacterial cells, their relevance to human health, and the specific medical conditions they treat. No matter if you're a student delving into the details of microbiology or a health professional seeking to refresh your knowledge, understanding the types of antibiotics and their applications plays a key role in achieving good health and combating formidable bacterial infections.
Antibiotics are a broad range of substances that are used to treat a variety of bacterial infections. Broadly categorized, antibiotics can be divided into many types, each with unique properties and uses.
Antibiotics can be categorized based on their chemical structure, the bacteria they target, and their mode of action. Let's delve deeper into some common types of antibiotics:
Penicillins are a group of widely used antibiotics that kill bacteria by breaking down their cell walls, leading to bacterial death.
Cephalosporins are a large group of antibiotics derived from the mould Acremonium (previously called Cephalosporium). They are grouped into generations based on their spectrum of antimicrobial activity.
| First Generation | Cefazolin, Cephalexin |
| Second Generation | Cefaclor, Cefuroxime |
| Third Generation | Ceftriaxone, Ceftazidime |
| Fourth Generation | Cefepime |
| Fifth Generation | Ceftaroline, Ceftobiprole |
Macrolides are a class of antibiotics derived from Streptomyces bacteria. They inhibit protein synthesis in bacteria by binding to the 50S subunit of the bacterial ribosome.
It's crucial to understand the different forms of antibiotics as they all have unique capabilities. Following are some more antibiotics explained.
Quinolones are broad-spectrum synthetic antibiotics that inhibit the DNA replication enzymes gyrase and topoisomerase IV.
Tetracyclines are a group of broad-spectrum antibiotics that inhibit protein synthesis by blocking the attachment of charged aminoacyl-tRNA to the A-site on the ribosome.
Aminoglycosides are powerful antibiotics used mainly to treat aerobic gram-negative bacilli infections. They work by binding to the bacterial 30S ribosomal subunit, causing misreading and interruption of the bacterial protein synthesis.
Sulfonamides inhibit the growth and multiplication of bacteria by acting as competitive inhibitors of p-aminobenzoic acid in the folic acid metabolism cycle.
Antibiotics work by attacking different aspects of bacterial physiology such as cell wall synthesis, protein synthesis, nucleic acid synthesis, and metabolic pathways. Let's explore some typical mechanisms of action:
Antibiotics that inhibit cell wall synthesis aim to disrupt the bacterial cell wall, leading to bacterial death. Penicillins and cephalosporins are classic examples of this type. They bind to PBPs (penicillin-binding proteins) and inhibit the final step in the synthesis of peptidoglycan, a component of the bacterial cell wall.
These antibiotics inhibit bacterial protein synthesis by acting on the ribosomes, the protein factories within the cell. Examples include tetracyclines, macrolides, and aminoglycosides.
Some antibiotics inhibit DNA and RNA synthesis by binding to DNA gyrase or DNA topoisomerase, enzymes involved in DNA replication and transcription. Quinolones and rifamycins are nucleic acid synthesis inhibitors.
These are antibiotics that inhibit essential metabolic processes within the bacterial cell, causing bacteria to starve to death. Examples include trimethoprim and sulfonamides, which inhibit the folic acid metabolism, crucial for cell growth and multiplication.
Understanding the different types of antibiotics and their uses can help you appreciate their significant role in medical science. Each antibiotic category is designed to treat specific infections and health conditions. This precision in the application of antibiotics contributes to their potency in eliminating or controlling bacterial growth.
Antibiotics are prescribed based on the nature of infection and the specific bacteria causing it. Each type of antibiotic is effective against a unique set of bacteria. Let's discuss the medical conditions that can be addressed using penicillins, cephalosporins, and macrolides.
Penicillins are derivatives of 6-aminopenicillanic acid and are used to treat bacterial infections caused by susceptible, usually gram-positive, organisms.
Cephalosporins are a large group of antibiotics that share a core structure with penicillins and thus possess similar mechanism of action, i.e., disrupting cell wall synthesis.
Macrolides inhibit protein synthesis in bacteria leading to their incapacity to reproduce and increase in number.
Antibiotics have an indispensable part in healthcare. Not only do they fight infections, but they also prevent potential health crises in vulnerable patients. Further, antibiotics like quinolones, tetracyclines, and aminoglycosides offer a wide range of health benefits.
Quinolones are synthetic antibacterial drugs that inhibit DNA gyrase and topoisomerase IV enzymes crucial for bacterial DNA replication and repair.
Tetracyclines, by binding to the bacterial 30S ribosomal subunit, inhibit protein synthesis leading to the cessation of bacterial growth.
Aminoglycosides, by binding to the 30S subunit of the bacterial ribosome, interfere with protein synthesis, thereby killing the bacteria.
Antibiotics are vital medical tools that combat bacterial infections in the body. Each antibiotic possesses a unique mode of action that targets different bacterial mechanisms or structures. To fully comprehend their functionality, it's key to understand how each type interacts with bacterial cells.
Antibiotics exhibit their effect by interacting with bacterial cells in several ways. These can broadly be grouped into two categories - bactericidal antibiotics that kill bacteria and bacteriostatic antibiotics that inhibit bacterial growth.
Antibiotics interact with bacterial cells through these primary mechanisms:
Let's delve deeper into how specific antibiotics like penicillins, cephalosporins, and macrolides interact with bacterial cells to bring about their actions.
Penicillins act as bactericidal antibiotics. The primary mode of action is the inhibition of cell wall synthesis.
More specifically, penicillins bind to proteins called penicillin-binding proteins (PBPs) located on the inner membrane of the bacterial cell wall. These proteins play a crucial role in the final step of cell wall synthesis - cross-linking the peptidoglycan chains. This process can be described by the formula:
\[ Cell \; Wall \; Synthesis \rightarrow Peptidoglycan \; Chains + PBPs \rightarrow Cross-linked \; Peptidoglycan \]By binding to the PBPs, penicillins block the cross-linking of peptidoglycan chains, leading to weaker cell walls that eventually burst due to the osmotic pressure difference across the wall.
Like penicillins, cephalosporins are also bactericidal and their mechanism of action involves the inhibition of bacterial cell wall synthesis.
They function by interfering with the synthesis of the peptidoglycan layer of bacterial cell walls. The peptidoglycan layer is important for cell wall structural integrity.
Cephalosporins bind to PBPs, prevent the cross-linking of peptidoglycan chains, and eventually cause the cell wall to rupture due to osmotic pressure resulting in the death of the bacteria. This mechanism can be illustrated using the same formula as for penicillins.
Macrolides perform their role majorly as bacteriostatic antibiotics. They inhibit bacterial growth by disrupting protein synthesis.
Macrolides are known to bind irreversibly to a site on the 50S subunit of the bacterial ribosome, thus inhibiting the translocation steps of protein synthesis. The specific reaction can be given by:
\[ Protein \; Synthesis \rightarrow Peptide \; Chains + tRNA \rightarrow Completed \; Proteins \]By inhibiting this process, macrolides prevent bacterial reproduction and increase their susceptibility to the immune system.
Through understanding how these antibiotics work at the molecular level, it becomes evident how crucial they are in treating bacterial infections and aiding the body's immune system.
Types of Antibiotics for Bacterial InfectionsAntibiotics are life-saving drugs primarily used to treat bacterial infections. Not only do they prevent bacteria from reproducing, but they can also directly kill these microorganisms. The manifold types of antibiotics, ranging from penicillins to quinolones, each play a vital role in managing different bacterial infections.
Before antibiotics are prescribed, several aspects are evaluated to ensure optimal outcomes and to maintain antibiotic efficacy for future use. Factors such as the type of bacteria, possible resistance, patient's allergic history, and antibiotic side-effects are carefully considered. Moreover, factors like dosage, duration of treatment, and potential interactions with other drugs are also taken into account.
In selecting antibiotics, doctors also consider the age, weight, and health status of the patient. For instance, pregnant women, infants, elderly individuals, or patients with renal or hepatic conditions may require different types of antibiotics or adjusted dosages. Finally, the cost and availability of the drug play a significant role, especially in low- and middle-income countries where antibiotic accessibility can be a challenge.
Quinolones are a type of antibiotic known for their broad-spectrum activity against both Gram-positive and Gram-negative bacteria.
Quinolones function as bactericidal drugs by inhibiting two essential enzymes in the bacterial DNA replication process, DNA gyrase and topoisomerase IV. This action blocks the cell's ability to synthesize DNA, thus preventing bacterial reproduction.
The general formula representing the action of quinolones can be represented as:
\[ DNA \; Replication \rightarrow DNA \; Strand + DNA \; Gyrase/Topoisomerase \; IV \rightarrow New \; DNA \; Strand \]By blocking the enzymes, the reaction halts, inhibiting bacterial growth. Quinolones such as ciprofloxacin and levofloxacin are commonly prescribed for treating infections such as pneumonia, urinary tract infections, and gastrointestinal infections.
Tetracyclines comprise another major class of antibiotics known for their deep penetration into bacteria and their versatile antimicrobial activity against many types of bacteria.
Tetracyclines primarily operate by inhibiting protein synthesis in bacteria. They attach to the 30S subunit of the bacterial ribosome, thus blocking the attachment of aminoacyl-tRNA to the mRNA-ribosome complex during protein synthesis. This action stops the addition of new amino acids to the peptide chain, disrupting the creation of essential proteins.
The action of tetracyclines can be described mathematically as:
\[ Protein \; Synthesis \rightarrow mRNA + Aminoacyl-tRNA \rightarrow Protein \]They effectively treat a wide range of conditions, such as acne, Lyme disease, and chlamydial infections. However, improper or overuse of tetracyclines can lead to bacterial resistance, reducing their effectiveness.
Aminoglycosides are potent antibiotics known for their effectiveness against severe infections caused by Gram-negative aerobic bacteria.
Aminoglycosides obstruct bacterial protein synthesis by binding to the 30S subunit of the bacterial ribosome. Their action results in the misreading of mRNA, which generates abnormal proteins that are non-functional and detrimental to the survival of the bacterium.
The action of aminoglycosides can be described as:
\[ Protein \; Synthesis \rightarrow mRNA + tRNA \rightarrow Abnormal \; Protein \]The aminoglycosides, such as gentamicin, can be used to treat severe infections caused by bacteria like Pseudomonas aeruginosa and Enterobacteriaceae. However, their use is often limited due to toxicity concerns.
How do Penicillins work?
Penicillins kill bacteria by breaking down their cell walls, leading to bacterial death. Common examples are Amoxicillin, Penicillin V and Penicillin G.
What is the mode of action of Quinolones?
Quinolones inhibit the DNA replication enzymes gyrase and topoisomerase IV. Common examples include Ciprofloxacin, Levofloxacin and Moxifloxacin.
How do antibiotics that inhibit cell wall synthesis work?
These antibiotics, like Penicillins and Cephalosporins, bind to PBPs (penicillin-binding proteins) and inhibit the final step in the synthesis of peptidoglycan, a component of the bacterial cell wall, leading to bacterial death.
Which antibiotic category is primarily used in treating infections such as Strep throat, Pneumonia, and Otitis media?
Penicillins are the type of antibiotics used to treat Strep throat, Pneumonia, and Otitis media. They work by inhibiting bacterial cell wall synthesis, leading to bacterial incapacity to survive.
For which health conditions are Macrolides commonly prescribed?
Macrolides are commonly prescribed for Community-acquired pneumonia, Uncomplicated skin infections, Pertussis (whooping cough), Diphtheria, and Chlamydia. They inhibit protein synthesis in bacteria, impacting their capability to reproduce.
What are the health benefits of antibiotics like Quinolones, Tetracyclines, and Aminoglycosides?
Quinolones are used for treating Urinary tract, Respiratory tract, Gastrointestinal, Bone and joint, and Skin and soft tissue infections. Tetracyclines manage Acne, Rosacea, Lyme disease, Chlamydia, Rickettsial infections and Anthrax. Aminoglycosides are used to treat Tuberculosis (as a second-line treatment), Sepsis, Respiratory tract infections, Complicated urinary tract infections, and Pelvic inflammatory disease.
Already have an account? Log in
Open in AppThe first learning app that truly has everything you need to ace your exams in one place
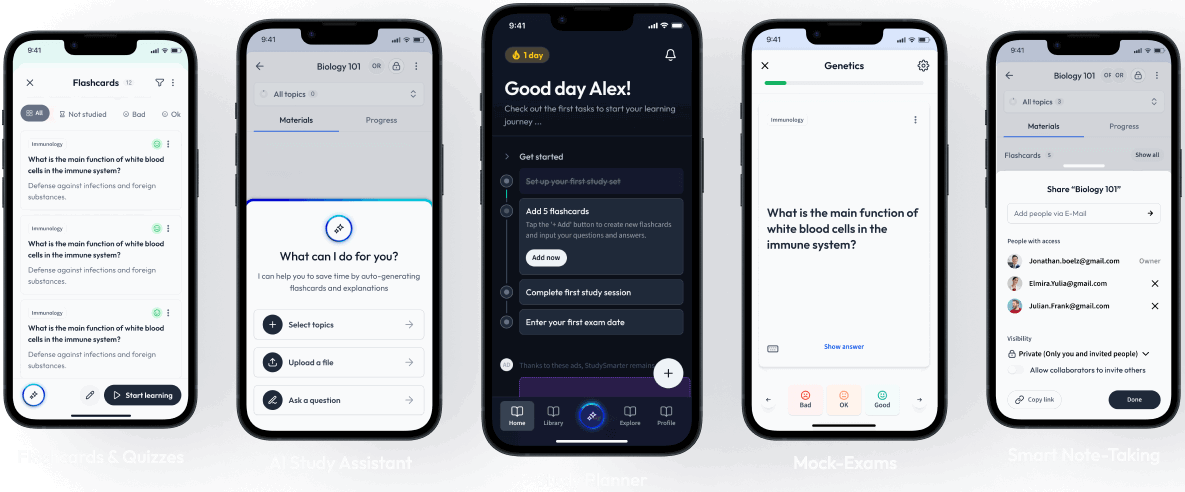
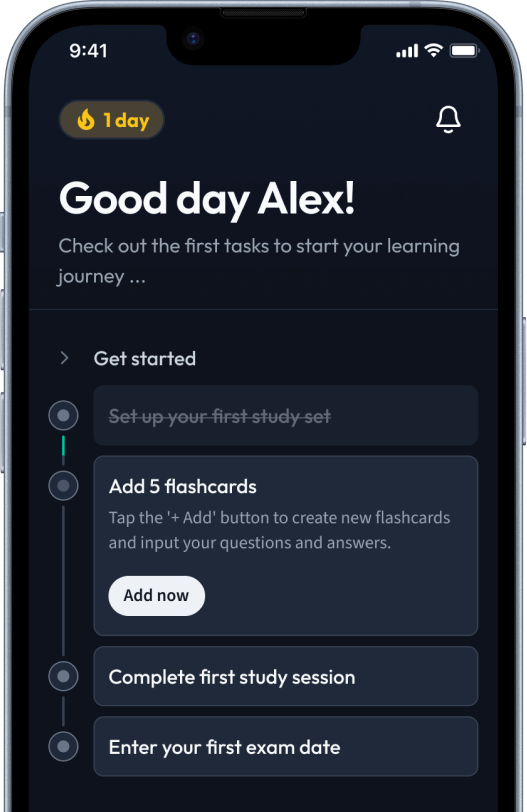
Sign up to highlight and take notes. It’s 100% free.
Save explanations to your personalised space and access them anytime, anywhere!
Sign up with Email Sign up with AppleBy signing up, you agree to the Terms and Conditions and the Privacy Policy of StudySmarter.
Already have an account? Log in