
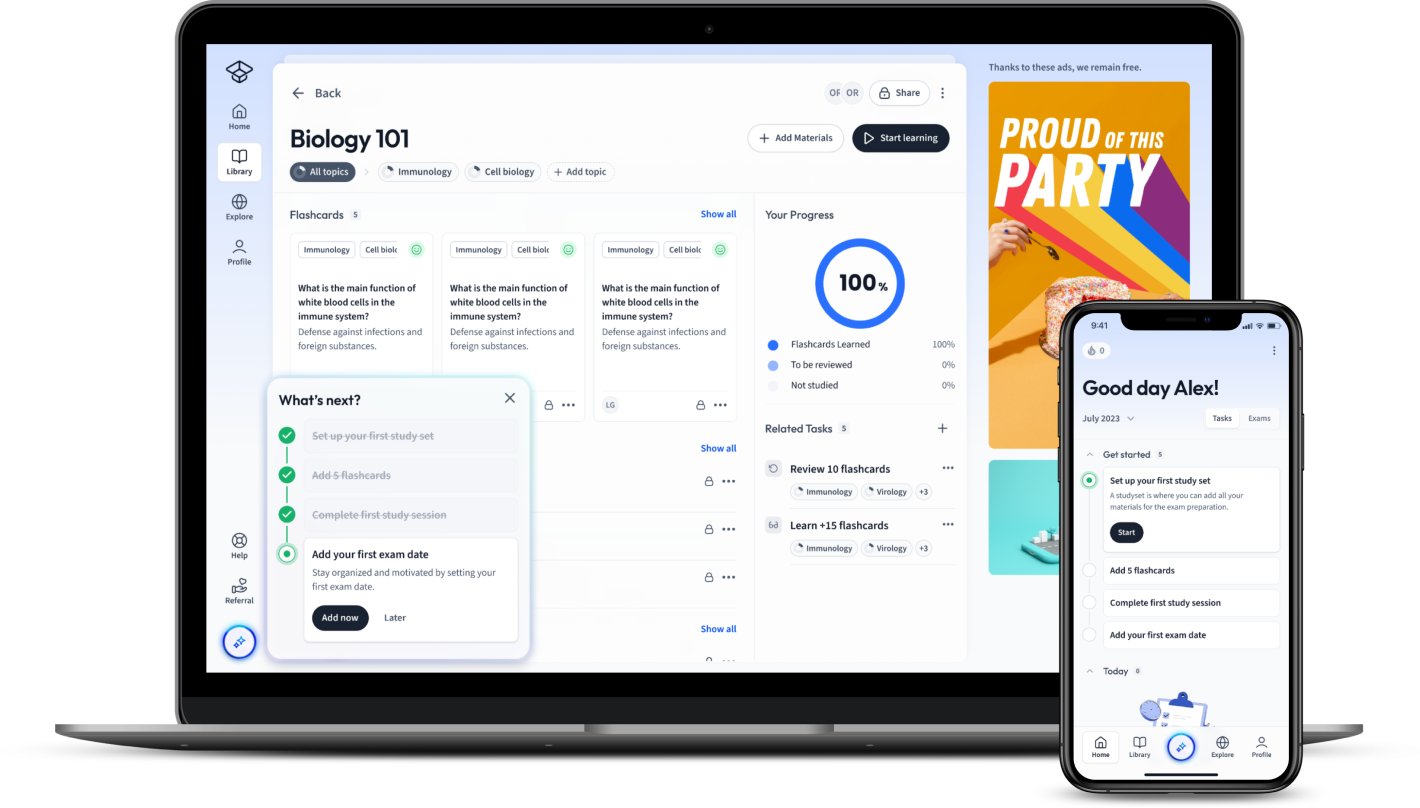
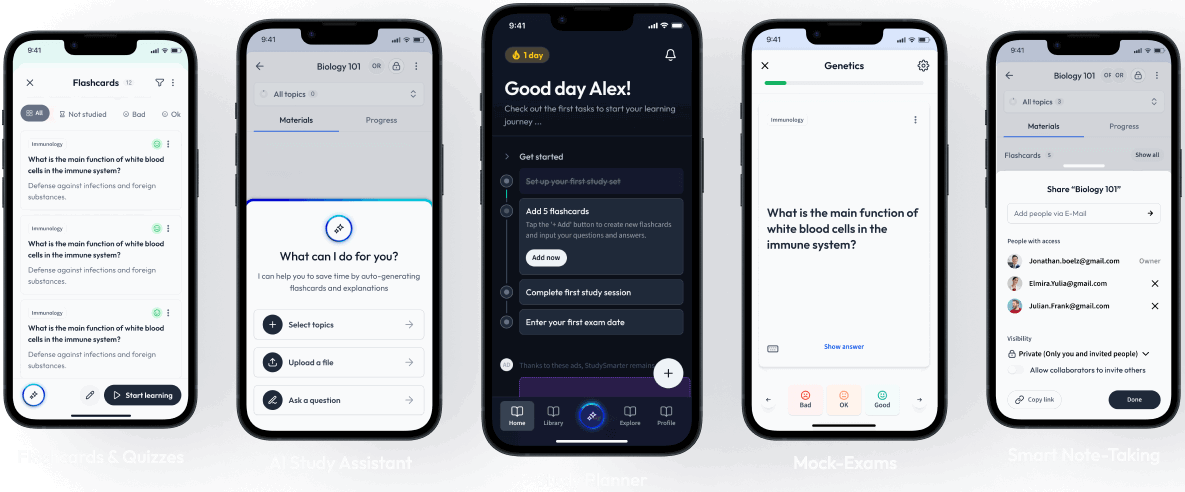
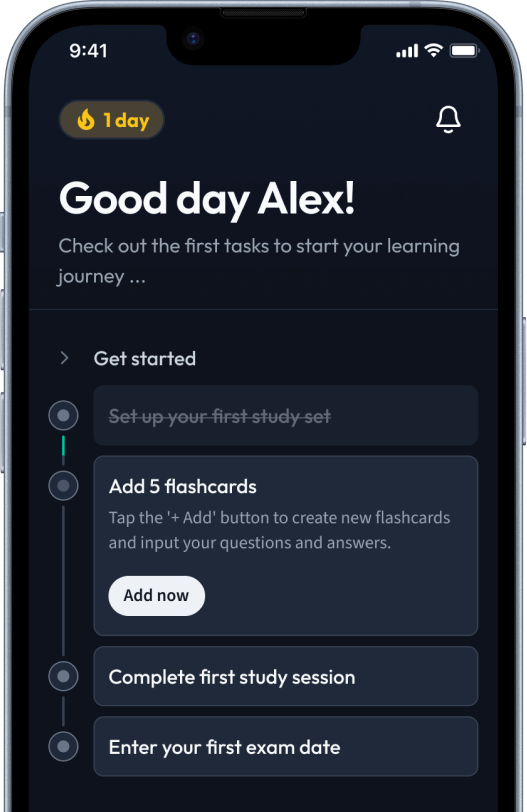
StudySmarter: Study help & AI tools
4.5 • +22k Ratings
More than 22 Million Downloads
Free
Navigate the complex landscape of immunisation with this comprehensive guide. Here, you'll find detailed information on the myriad types of vaccines, including active and passive immunisation, live-attenuated and inactivated vaccines, and much more. Learn about COVID-19 vaccines, flu vaccines, and other vaccinations, such as routine, travel, and seasonal vaccines, along with an exploration of bacterial vaccines. You'll also discover how these vaccines work, from antigen functions to immune responses, and wade into the various administration routes. This all-inclusive exploration aims to inform and educate on every corner of vaccine types and their uses.


Lerne mit deinen Freunden und bleibe auf dem richtigen Kurs mit deinen persönlichen Lernstatistiken
Jetzt kostenlos anmeldenNavigate the complex landscape of immunisation with this comprehensive guide. Here, you'll find detailed information on the myriad types of vaccines, including active and passive immunisation, live-attenuated and inactivated vaccines, and much more. Learn about COVID-19 vaccines, flu vaccines, and other vaccinations, such as routine, travel, and seasonal vaccines, along with an exploration of bacterial vaccines. You'll also discover how these vaccines work, from antigen functions to immune responses, and wade into the various administration routes. This all-inclusive exploration aims to inform and educate on every corner of vaccine types and their uses.
Vaccines play a vital role in the prevention of infectious diseases by training our immune system to fight harmful pathogens. Understanding how different types of vaccines work helps not only to comprehend this essential health tool more clearly, but also demystifies their immunological mechanics.
There is a wide range of vaccines with diverse types and mechanisms targeting different diseases. A broad understanding of these types is essential for appreciating how they protect you from various diseases. This section elaborates on the key types of vaccines including active and passive immunisation, as well as live-attenuated, inactivated, subunit, conjugate, toxoid, DNA, and recombinant vector vaccines.
Essentially, a vaccine is a biological preparation that provides active acquired immunity to a particular disease. It contains antigens that resemble disease-causing microorganisms and is often made from weakened or killed forms of the microbe, its toxins, or one of its surface proteins.
Active immunisation stimulates the body to produce an immune response to a specific infection. The body then remembers this immune response, which is faster and more effective if the person is ever exposed to the same disease again.
On the other hand, passive immunisation provides short-term protection by giving antibodies that are taken from a donor directly to your body.
A classic example of active immunisation is the Measles, Mumps, and Rubella (MMR) vaccine, which strengthens the immune system by building antibodies against these diseases. In contrast, an example of passive immunisation is the use of rabies immune globulin, where the person is given direct anti-rabies antibodies after being bitten by a rabid animal.
Live-Attenuated Vaccines contain a live, but weakened version of a virus or bacteria. These vaccines mimic a natural infection, stimulating a strong immune response. They are often effective with a single dose.
Inactivated Vaccines, however, are made from viruses or bacteria that have been killed or inactivated. These vaccines often require multiple doses over time (booster shots) to maintain immunity.
An example of a live-attenuated vaccine is the Yellow Fever Vaccine, while the Hepatitis A vaccine is an example of an inactivated vaccine.
Subunit, Conjugate, and Toxoid Vaccines use specific pieces of the virus or bacteria — like its protein, sugar, or capsid (a casing around the virus). Since these vaccines use only specific pieces, they give a very strong immune response that’s targeted to key parts of the organism.
Furthermore, Conjugate vaccines are a type of subunit vaccine that are designed to produce a stronger immune response. They do this by linking an additional protein to the antigen in order to enhance the immune response.
Finally, Toxoid vaccines are used against bacteria that produce toxins. These vaccines are designed to target the toxins produced by the bacteria rather than the bacteria themselves.
The HPV vaccine is an example of a subunit vaccine, while the HIB vaccine used to protect against Haemophilus influenzae type b is an example of a conjugate vaccine. The Tetanus vaccine is an example of a toxoid vaccine.
DNA vaccines use the gene of a virus or bacteria to stimulate an immune response. Unlike other vaccines, this type does not use pathogens or proteins. Instead, it introduces a DNA sequence encoding the antigen.
Recombinant Vector Vaccines, are a type of genetic engineering where genetic material from a disease-causing organism is inserted into a 'vector' – a virus or bacteria that doesn't cause disease. This produces an antigen, triggering an immune response.
Fascinatingly, the COVID-19 vaccines developed by AstraZeneca (AZD1222) and Johnson & Johnson (Janssen) are examples of vector vaccines. They have innovatively harnessed the power of biotechnology to prevent disease in a new and unique way.
In the fight against the coronavirus pandemic, various types of COVID-19 vaccines have been developed, with each employing a unique strategy to stimulate an immune response against the SARS-CoV-2 virus. Here, we delve into the details of mRNA-based and viral vector-based COVID-19 vaccines, focusing in particular on vaccines from Pfizer-BioNTech, Moderna, Johnson & Johnson's Janssen, and Oxford-AstraZeneca.
mRNA-based vaccines represent a novel approach to immunisation. Unlike traditional vaccines that introduce inactivated or attenuated virus into the body, mRNA vaccines carry the genetic instructions that cells use to make the virus's distinctive spike protein. The immune system then generates a response to these proteins, providing immunity to the virus. This section will dissect the specifics of the Pfizer-BioNTech and Moderna vaccines.
The Pfizer-BioNTech vaccine, officially known as BNT162b2, is an mRNA vaccine. The 'm' in mRNA stands for 'messenger', and this vaccine works by sending a message into your body that instructs your cells to produce a harmless piece of the spike protein found on the surface of the SARS-CoV-2 virus.
Once these spike proteins are produced, your immune system is triggered to produce an immune response. This creates memory cells that will recognise and respond to the protein if the actual virus ever invades your body.
| Vaccine Name: | Pfizer-BioNTech |
| Technology: | mRNA |
| Dosage: | 2 Doses, 21 Days Apart |
| Efficacy: | Around 95% |
Efficacy refers to the performance of an intervention under ideal and controlled circumstances, such as during a clinical trial.
Similar to the Pfizer-BioNTech version, the Moderna COVID-19 vaccine is also an mRNA vaccine that works by instructing cells in the body to produce a piece of the spike protein of the SARS-CoV-2 virus. This provokes an immune response, producing antibodies and developing immune memory, preparing the body to fight off the virus if exposed in the future.
An interesting point to note about the Moderna vaccine is that it does not need to be stored at ultra-cold temperatures, unlike its Pfizer-BioNTech counterpart. This makes it a more viable option for areas without advanced cold storage facilities.
| Vaccine Name: | Moderna |
| Technology: | mRNA |
| Dosage: | 2 Doses, 28 Days Apart |
| Efficacy: | Around 94.1% |
Unlike mRNA-based vaccines, viral vector vaccines use a harmless virus, different from the coronavirus, to deliver a piece of the SARS-CoV-2 virus to our cells, leading to a protective immune response. The Johnson & Johnson's Janssen and Oxford-AstraZeneca vaccines employ this technology.
The Johnson & Johnson's Janssen COVID-19 Vaccine employs a viral vector-based approach. It uses a harmless adenovirus to deliver a piece of the DNA from the SARS-CoV-2 virus.
When the SARS-CoV-2 DNA is inside our cells, it provides instructions to make the virus's spike protein. Our immune system then learns to recognize and fight the virus should we encounter it in the future.
| Vaccine Name: | Johnson & Johnson's Janssen |
| Technology: | Viral Vector |
| Dosage: | Single Dose |
| Efficacy: | Around 66.3% |
The Oxford-AstraZeneca Vaccine, also viral vector-based, uses a version of a common cold virus (adenovirus) from chimpanzees, modified so it can’t cause disease in humans. Like the Johnson & Johnson vaccine, the AstraZeneca vaccine delivers the SARS-CoV-2 spike protein to our cells to instigate an immune response.
This vaccine has the advantage of being able to be stored at normal fridge temperature, making it easier to distribute, especially in developing countries.
| Vaccine Name: | Oxford-AstraZeneca |
| Technology: | Viral Vector |
| Dosage: | 2 Doses, 4-12 Weeks Apart |
| Efficacy: | Around 62% |
Adenovirus is a group of related viruses that cause illnesses like the common cold, sore throat, bronchitis, pneumonia, diarrhoea, and pink eye.
Exploring the different flu vaccines can provide essential insights into how science has diversified its approaches towards one common goal – effective prevention of influenza. Let's delve deeper into Inactivated Influenza Vaccines (IIV), Live Attenuated Influenza Vaccine (LAIV) and Recombinant Influenza Vaccine (RIV).
Inactivated Influenza Vaccines, known as IIVs, are designed to help prevent the flu. Such vaccines contain inactivated or 'killed' influenza viruses, and are administered via injection. There are significant differences within this category, particularly when comparing standard-dose and high-dose vaccines.
The Standard Dose Influenza Vaccines are commonly administered for seasonal flu prevention. These vaccines contain three influenza virus strains (trivalent) or four strains (quadrivalent). These strains include influenza A (H1N1) virus, influenza A (H3N2) virus and one or two influenza B viruses.
A standard-dose flu shot for adults contains 15 micrograms (\( \mu g \)) of hemagglutinin (HA) per virus strain. The influenza viral HA is the primary target for the immune system's response, and the amount of HA in a vaccine is a key factor in its effectiveness.
Approved standard-dose trivalent flu shots for the 2021-2022 season, for instance, include Fluvirin, Afluria and Fluarix.
Moving onto the High Dose Influenza Vaccines, these are often considered for older adults (65 years and over) who are at higher risk of severe influenza illness and complications. As the name implies, they contain a higher dose of antigen, aiming to induce a stronger immune response.
For example, the high-dose trivalent flu vaccine, Fluzone High-Dose, contains 60 micrograms (\( \mu g \)) of HA per virus strain, four times the dosage found in standard vaccines.
In recognition of the higher risk of influenza complications in seniors, the NHS offers a high-dose flu vaccine, FLUAD®, to all individuals over 65.
The Live Attenuated Influenza Vaccine (LAIV) is significantly different from IIVs in that it contains live influenza viruses that have been 'attenuated', meaning they have been weakened. This way, the viruses induce an immune response without causing disease. This type of vaccine is administered through a nasal spray rather than an injection.
Due to its live, weakened viruses, the LAIV is recommended only for healthy, non-pregnant individuals aged 2-49 years. Theoretically, the body's immune response to the live vaccine may more closely resemble the response to a natural influenza infection, potentially providing better immunity.
The standard dosage for LAIV is 0.2 milliliters, split between the two nostrils. Major brands for the LAIV include Fluenz Tetra in the UK and FluMist Quadrivalent in the US.
Last, but certainly not least, is the Recombinant Influenza Vaccine (RIV), the newest form of influenza vaccine. Unlike traditional flu vaccines, RIVs are produced without the need for eggs, making it a suitable choice for individuals with egg allergies.
RIVs are produced by combining proteins from the virus with parts of another virus that can grow in cells in a lab. This engineered 'composite' virus then grows and produces virus proteins that stimulate a protective immune response, but it doesn't produce the flu.
FluBlok Quadrivalent is the only RIV approved as of now, approved for people 18 years and older. Just like high-dose influenza vaccines, RIVs contain 45 \( \mu g \)) of HA per virus strain, significantly higher than standard IIVs.
The development and availability of these diverse types of vaccines is a testament to the science of immunology, and how it evolves to meet public health needs better.
There are several different types of vaccinations designed to help protect against a range of illnesses and diseases. As such, vaccinations can be classified into various categories, such as routine vaccinations, travel vaccinations, and seasonal vaccinations. Each category serves a different purpose and targets various populations.
Routine vaccinations constitute a significant part of preventive healthcare. They are typically divided into two categories: those meant for children and those designed for adults.
A child's immune system requires vaccination against a slew of serious and potentially life-threatening diseases. The UK childhood immunisation schedule starts at 8 weeks of age and includes vaccinations against diseases such as measles, mumps, and rubella (MMR), diphtheria, whooping cough, and tetanus.
Adults too need routine vaccinations, which not only protect the individual but also contribute to herd immunity, protecting others in the community who cannot receive certain vaccines. The UK schedule includes vaccines for diseases like flu and pneumococcal disease.
Vaccination before travelling is essential to protect individuals from contracting diseases that are less common in the UK. Depending on the country or region you're visiting, different vaccinations might be recommended. Some countries may also require proof of certain vaccinations for entry. Hepatitis A, Typhoid, and Yellow Fever are examples of vaccines may be required or recommended for certain overseas travels.
Seasonal vaccinations are designed to protect against diseases that are most common during specific times of the year. The most well-known examples of this are influenza vaccinations, often known as flu jabs, which are typically given in the autumn and winter seasons when flu viruses are most active.
The flu vaccine changes every year to cover the flu viruses that are most likely to circulate in the coming season. Information about these expected viruses is gleaned through global surveillance and advanced scientific forecasting. This annual reformulation of the flu vaccine is essential since influenza viruses continually evolve.
When looking at the vast world of vaccines, bacterial vaccines form a major part. Each bacterial vaccine has its unique formulations and works against specific bacteria to prevent diseases. Selected important ones include the Tuberculosis (BCG) Vaccine, the Diphtheria, Tetanus, and Pertussis (DTaP) Vaccine and the Haemophilus Influenzae type b (Hib) Vaccine.
The BCG vaccine provides immunity against tuberculosis (TB), a serious infection that primarily affects the lungs but can affect other parts of the body as well. TB is caused by the bacterium Mycobacterium tuberculosis.
The BCG vaccine is given to those at higher risk of TB. In the UK, the vaccine is usually offered to babies who are born in areas where TB rates are high, or to those with parents or grandparents hailing from a country with high TB rates.
The BCG vaccine is administered as a single injection into the upper arm. It can cause minor side effects such as fever, a sore arm, and swollen glands. More rarely, it can result in a severe skin reaction or a swollen gland in the armpit or neck.
The vaccine's effectiveness varies from 60% to 80%, and it's most effective against severe forms of TB, like TB meningitis in children. Contrary to some beliefs, BCG does not always prevent against TB in lungs, which is the most common form of TB in adults.
The DTaP vaccine protects against three life-threatening bacterial diseases: Diphtheria, Tetanus, and Pertussis (whooping cough). All three diseases are caused by bacteria: Corynebacterium diphtheriae causes Diphtheria, Clostridium tetani causes Tetanus, and Bordetella pertussis causes Pertussis.
This combination vaccine is among the first vaccines given to infants and children. In the UK, the DTaP vaccine is combined with vaccines against polio, Hib, and Hepatitis B (commonly referred to as the 6-in-1 vaccine) and is given to babies at 8, 12, and 16 weeks of age.
Diphtheria, Tetanus, and Pertussis are all severe diseases leading to serious health issues or even death. Diphtheria and Pertussis spread from person to person, while Tetanus enters the body through cuts or wounds.
Diphtheria:This bacterial infection could lead to severe respiratory issues, heart problems, nerve damage, or even death.
Tetanus (Lockjaw): Tetanus causes painful muscle tightening and stiffness, leading to severe health issues like 'locking' of the jaw prohibiting the patient from opening their mouth or swallowing.
Pertussis (Whooping Cough):Pertussis causes severe coughing spells, difficulty in breathing, vomiting, disturbed sleep, weight loss, incontinence, and, in infants, the symptoms can be more severe and possibly fatal.
The Hib vaccine offers protection against infection caused by Haemophilus influenzae type b, a bacterium that can lead to severe illnesses like meningitis, pneumonia, and sepsis, particularly in young children.
In the UK, the Hib vaccine is offered to babies at 8, 12, and 16 weeks along with the 6-in-1 vaccine (just like the DTaP vaccine). Also, a booster dose is given when the child is one year old to provide longer-term protection. An additional catch-up jab may also be offered to some older children and adults who are at risk of the disease.
Before Hib vaccines were introduced, Hib used to be a significant cause of bacterial meningitis. However, since the introduction of Hib vaccines, the number of cases of severe Hib diseases has decreased considerably. This demonstrates the practical effectiveness of the Hib vaccine.
The microorganism Haemophilus influenzae got its name because it was originally thought to cause influenza. However, we now know that this isn't the case. "Hib" is a type of Haemophilus influenzae that causes severe disease.
Unravelling the mechanism of how vaccines work is a fascinating journey into the complex world of immunology. Vaccines cleverly utilise the body's natural defence system – the immune system to protect us from harmful pathogens. Let's delve into this journey, starting with the role of antigens in stimulating an immune response.
Vaccines work by mimicking disease agents and stimulating the immune system's response. They do so without causing the disease itself. Vaccines are typically formulated from the same germs (or parts of them) that cause the disease. For instance, this can be a live but weakened or attenuated germ, dead or inactivated germ, or a component of the germ, like its proteins or sugars.
When the vaccine containing these elements is administered, the human immune system recognises them as foreign invaders, or antigens. The immune system mounts an attack against these antigens by producing proteins called antibodies. These antibodies neutralise, eliminate, or bring about the destruction of the antigens.
After the threat is neutralised, some of the cells that were involved in the production of antibodies persist in the body. These cells, known as memory cells, remain 'on stand-by,' ready to respond if the body encounters the real disease-causing germ in the future. If that happens, the memory cells produce antibodies much more quickly. This rapid response can either prevent the disease altogether or make it less severe.
Antigens play a crucial role in vaccine development and lend to vaccine's effectiveness. They are substances that appear foreign to the immune system and trigger the immune response. These antigens are included in vaccines to mimic disease-causing microorganisms. Essentially, they trick the immune system into producing an immunological response, that being the production of antibodies.
In most vaccines, these antigens won't cause disease themselves. They've been either killed or weakened to a point that they do not pose any risk. However, their presence is enough to arouse the immune system, instigating the immune response that'll help to protect against future infections.
Antigens: These can be proteins, sugars, or any component of the pathogen or the pathogen itself that the immune system recognises as foreign and responds to.
After the primary immune response to a vaccine, some of the memory cells that are produced persist long-term in the body. These cells remember the antigen that stimulated the initial immune reaction. If the pathogen were ever to attempt invasion again, these memory cells could recognise it and rapidly produce a wave of targeted antibodies, often before the pathogen could cause disease, resulting in acquired immunity.
Memory Cells: These are the components of the immune system that 'remember' the antigens they have previously encountered, enabling a faster response to subsequent infections.
Through this process, vaccines protect individuals. However, they also contribute to a broader public health goal known as herd immunity (or community immunity). Herd immunity occurs when a high percentage of a population is immunised. This helps to prevent the spread of infectious diseases, decreasing the likelihood of an outbreak and protecting those unable to get vaccinated (like those with severe allergies or immune system disorders).
Not all vaccines rely on the same mechanism to trigger an immune response. Indeed, the differences in vaccine types typically come down to how they interact with the immune system to provoke this response. Here, let's examine how live-attenuated vaccines and the more recent mRNA vaccines work.
Live-attenuated vaccines are made from a version of the living virus or bacterium that has been weakened (or 'attenuated') in the lab. Some examples include Measles, Mumps, and Rubella (MMR) vaccine, and the Varicella (chickenpox) vaccine. Because they contain the live pathogen, albeit weakened, these vaccines stimulate a strong and long-lasting immune response. Just 1 or 2 doses of a live vaccine can give you a lifetime of protection against a germ and the disease it causes.
However, live vaccines aren't suitable for everyone. They are not given to people with weakened immune systems, long-term health conditions, or those who are pregnant.
The most recent entrants into the vaccine toolkit are mRNA vaccines such as the Pfizer-BioNTech and Moderna vaccines for COVID-19. Instead of using live or inactivated virus, mRNA vaccines deliver a tiny piece of the virus's genetic material (its mRNA) into human cells. This prompts the cells to produce a viral protein, which the immune system then recognises and responds to.
mRNA vaccines have displayed robust ability to stimulate both the antibody production and cell-mediated immunity, offering protection against disease. However, maintaining the stability of mRNA molecules poses significant challenges due to their tendency to degrade rapidly.
mRNA Vaccines: These are vaccines that work by introducing a piece of mRNA from the pathogen to trigger an immune response.
Overall, the world of vaccines is complex and varied, and these are just a few examples illustrating how different vaccines work to keep us safe.
Vaccines, as powerful health tools, are administered through a variety of routes to improve their effectiveness and tolerability. This section will explore the primary methods of vaccine administration.
Intramuscular vaccination is a common method where the vaccine is injected directly into the muscle, typically in the upper arm (deltoid muscle) for adults and the thigh (anterolateral thigh muscle) for infants and young children.
The intramuscular route has several advantages. Firstly, because muscles have a rich blood supply, the vaccine is absorbed quickly and effectively. Secondly, muscle tissue tends to experience less pain and irritation in response to a vaccine, compared to subcutaneous tissue.
However, there are also potential complications. Incorrect IM injection could result in local trauma, muscle fibre damage, or nerve injury. Therefore, a trained healthcare worker with knowledge of precise anatomical landmarks is essential for proper IM vaccination.
Most vaccines, such as Hepatitis B, Influenza, and Pneumococcal vaccines, are administered via this route.
Unlike intramuscular injections, subcutaneous vaccinations are injected into the fat layer beneath the skin but above the muscle. The usual sites for subcutaneous injections are the fatty parts of the upper arm, abdomen, or thigh.
Subcutaneous injections are generally used when slower absorption rates of the vaccine are needed. Also, since the subcutaneous layer has fewer blood vessels compared to muscles, they are less likely to cause a bleeding event, especially for individuals on anticoagulant therapy.
Subcutaneous vaccination also has potential complications, such as skin and fat layer atrophy (thinning), or local infection. The Measles-Mumps-Rubella (MMR), Varicella and Zoster vaccines are typical examples of vaccines given via subcutaneous injection.
The intradermal vaccination involves injection of the vaccine into the dermis, the skin layer below the epidermis and above the subcutaneous tissue. This is the shallowest injection among all methods of parenteral (non-oral) administration.
The human skin, rich in immune cells, allows for efficient interaction of the vaccine with the immune system. As such, intradermal vaccination often requires less vaccine dosage compared to intramuscular or subcutaneous, while still eliciting a comparable immune response.
The challenge of the intradermal route is the higher skill needed for injection, as it requires a precise technique to ensure correct placement of the vaccine. The Bacille Calmette-Guérin (BCG) and some forms of influenza vaccines are examples of vaccines administered via the intradermal route.
Rather than using injections, oral vaccines are consumed through the mouth. This offers several advantages, such as ease of administration, making it an ideal method especially in large-scale immunisation campaigns.
Moreover, oral vaccines assist in stimulating the mucosal immune system - the immune response at the site where the infection enters the body. This can lead to better protection against some diseases that enter the body through mucous membranes, such as the gut or respiratory tract.
However, oral vaccines aren't suitable for all types of diseases. They are typically used for diseases caused by pathogens that invade the body via the gastrointestinal tract. Examples of oral vaccines include the polio (Sabin), rotavirus, and typhoid vaccines. Understanding these various methods of administration helps to understand how vaccines reach the immune system and thereby elicit an effective response. The route of administration can also affect factors such as how quickly the vaccine takes effect, how long immunity lasts, and potential side effects.
What are the four types of vaccines mentioned and how do they work?
The four types of vaccines are: live, attenuated vaccines, which contain weakened versions of the virus or bacteria; inactivated vaccines, where the germ has been killed; subunit, recombinant, polysaccharide, and conjugate vaccines, that use specific parts of the germ; and toxoid vaccines, which use inactivated toxins from bacteria.
What is the function of vaccines in the body?
Vaccines stimulate your body's immune response, helping you fight off specific infectious diseases. They contain elements from the disease-causing organism to stimulate an immune response and provide immunity against the diseases.
What is an example of an inactivated vaccines and what is it used for?
An example of an inactivated vaccine is the Hepatitis A vaccine. It is used to stimulate an immune response against Hepatitis A, a liver disease caused by the Hepatitis A virus.
What are the three primary types of flu vaccines?
The three primary types are Trivalent vaccines, Quadrivalent vaccines, and High-Dose vaccines.
Why is the flu vaccine formulated annually?
The flu vaccine is prepared annually to match the expected strains of the flu virus for that year, which continually evolves.
What is the main purpose of flu vaccines and what are its broader impacts?
The main purpose of flu vaccines is to reduce the risk of illness due to the flu. They also reduce the severity of disease, decrease the risk of hospitalisation, and promote 'herd immunity'.
Already have an account? Log in
Open in AppThe first learning app that truly has everything you need to ace your exams in one place
Sign up to highlight and take notes. It’s 100% free.
Save explanations to your personalised space and access them anytime, anywhere!
Sign up with Email Sign up with AppleBy signing up, you agree to the Terms and Conditions and the Privacy Policy of StudySmarter.
Already have an account? Log in